Cancers in general
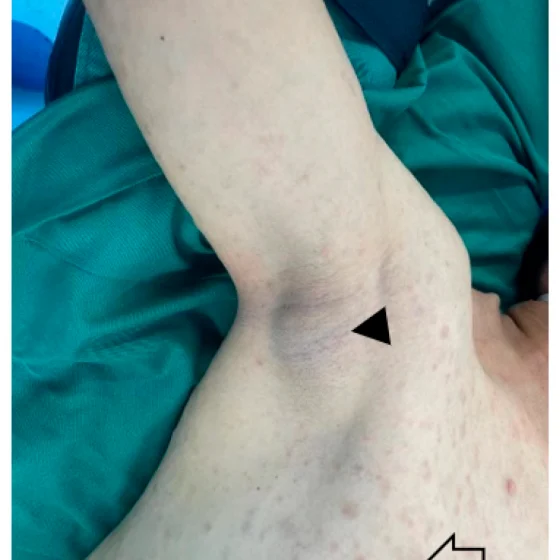
Kaposi’s sarcoma
Kaposi’s sarcoma (KS) is a rare type of soft tissue sarcoma. A soft tissue sarcoma is a type of cancer. What is Kaposi’s sarcoma? Kaposi’s sarcoma (KS) develops from cells called endothelial cells, which line the blood and lymph vessels. It is most commonly found on the skin, but it can also affect the inside of the body, such as the lymph nodes, lungs, bowel, liver and spleen. KS growths are also called lesions or tumours. KS develops in a different way from other types of cancer. Most cancers begin in one place in the body and may then spread to
Treatment for Large bowel and rectal neuroendocrine tumours (NETs)
The treatment you have for a large bowel or rectal neuroendocrine tumour (NET) depends on a number of factors. This includes where the cancer started, its size and whether it has spread (the stage). Surgery is the main treatment for large bowel and rectal NETs and is usually the only treatment that can cure it. Which treatment do I need? A team of doctors and other professionals discuss the best treatment and care for you. They are called a multidisciplinary team (MDT). The treatment you have depends on: where the large bowel or rectal NET started and its size whether
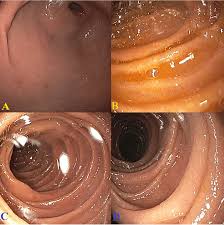
Linitis plastica of the stomach
Gastric linitis plastica is the medical term for a rare type of stomach (gastric) cancer. It can thicken your stomach wall and affect digestion. Treatment for linitis plastica is like treatment for other types of stomach cancers. What is linitis plastica? Linitis plastica is a type of adenocarcinoma. Adenocarcinoma is the most common form of stomach cancer. Linitis plastica spreads to the muscles of the stomach wall and makes it thicker and more rigid. This means that the stomach can’t hold as much and doesn’t stretch or move as it should when you’re digesting food. This stiff walled stomach is sometimes
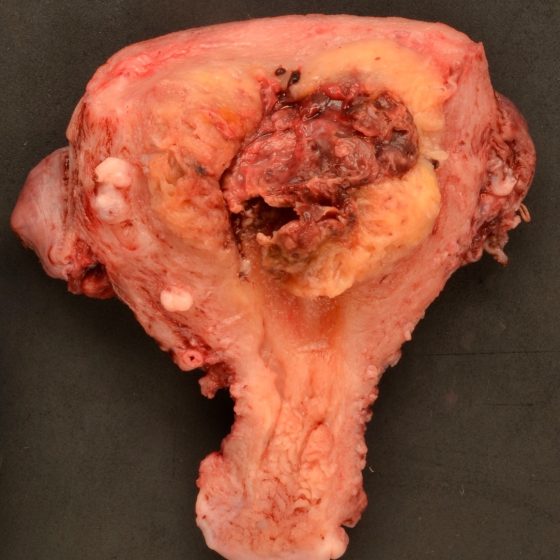
Malignant peripheral nerve sheath tumor (MPNST)
Malignant peripheral nerve sheath tumours (MPNSTs) is rare. It is a type of peripheral nerve sheath tumour that is cancerous (malignant). Most peripheral nerve sheath tumours are not cancerous (benign). A tumour is a lump or growth in the body. One type of non cancerous peripheral nerve sheath tumour is called a schwannoma. What is a malignant peripheral nerve sheath tumour? Malignant peripheral nerve sheath tumours are a type of peripheral nerve sheath tumour. These cancers begin in the layer (nerve sheath) that cover the peripheral nerves. Peripheral nerves send messages between the brain and spinal cord and the rest
Mediastinal germ cell tumours
The mediastinum is the area in the centre of the chest, between the lungs. It is pronounced media-sty-num. Mediastinal germ cell tumours are a type of tumour that grow in the mediastinum. They develop in a type of cell called germ cells. There are different types of mediastinal germ cell tumours. Some mediastinal germ cell tumours are non cancerous (benign). Your treatment depends on what type of mediastinal germ cell tumour you have. Treatment options include surgery and chemotherapy. What are mediastinal germ cell tumours? Germ cell tumours develop in germ cells. These are the cells in the body that develop into
Merkel cell carcinoma (MCC)
Merkel cell carcinoma (MCC) is a rare type of skin cancer. It starts in the Merkel cells, which are usually in the top layer of the skin (the epidermis). These cells are near the nerve endings and they help us respond to touch. MCC is very rare. Just over 1,500 people were diagnosed with MCC in England between 1999 and 2008. Because Merkel cells are a type of neuroendocrine cell, MCC is also called a neuroendocrine tumour (NET) of the skin. Risks and causes of MCC There are some factors that increase your risk of developing Merkel cell carcinoma (MCC).
Treatments for neuroblastoma
Doctors plan your child’s treatment in one of the major children’s cancer centres. Your child has most of their treatment in this specialist centre. They might have some care at a hospital closer to home. Children’s cancer centres have teams of specialists who know about neuroblastoma and the best way to treat them. The main treatments include: surgery chemotherapy radiotherapy immunotherapy Decisions about treatment The specialist team plan treatment based on several factors, including your child’s age. Your child’s treatment depends on their risk group. A pathologist looks at the neuroblastoma cells under a microscope. This along with the scans and other
Treatment for phaeochromocytomas
The main treatment for phaeochromocytoma is surgery. Other treatments include internal radiotherapy, external radiotherapy and chemotherapy. Your treatment depends on different factors including: the size of the tumour whether it has spread your general health and fitness A team of doctors and other professionals discuss the best treatment and care for you. They are called a multidisciplinary team (MDT). The team usually includes a: specialist surgeon doctor specialising in hormone disorders (endocrinologist) cancer doctor (oncologist) doctor specialising in the diseases of tissues or cells (pathologist) doctor specialised in reading scans (radiologist) clinical nurse specialist (CNS) You may need to travel
Treatment for pseudomyxoma peritonei
The main treatments for pseudomyxoma peritonei (PMP) are surgery and chemotherapy. Your treatment depends on the size of the cancer and your general health. You might not start treatment straight away. Your doctor closely monitors your cancer in case you need treatment in the future. This is called watch and wait. If you need treatment you might have: surgery combined with chemotherapy into the tummy (abdomen) surgery to remove as much cancer as possible (debulking surgery) chemotherapy Watch and wait Your doctor might decide to closely monitor your cancer if it’s small and slow growing and you don’t currently need
Treating retinoblastoma
Retinoblastoma is rare and so your child will go to a specialist centre for treatment. There are different treatments such as freezing and laser therapy, chemotherapy, radiotherapy and surgery. The treatment your child has depends on several things including the size of the cancer and if it is in one or both eyes. Treatment centres There are 2 specialist retinoblastoma centres in England and they are: The Royal London Hospital Birmingham Children’s Hospital These 2 centres serve all parts of the UK including Wales, Scotland and Northern Ireland. They have teams of specialists who know a lot about retinoblastoma and
Treatment for small bowel cancer
Your treatment will depend on what type of small bowel cancer you have. This page is about the treatment you might have if you have small bowel adenocarcinoma. This is the most common type of small bowel cancer. Treatment for other types of small bowel cancer, such as neuroendocrine tumours and lymphoma will be different. Deciding which treatment you need Your doctor will talk to you about the treatment they suggest. They will explain its benefits and the possible side effects. Your treatment will depend on: where your cancer is how big it is and whether it has spread (the stage) the type
Treatment for small bowel neuroendocrine tumours
The treatment you have depends on a number of things. This includes where the cancer started, its size and whether it has spread (the stage). Surgery is the main treatment for small bowel neuroendocrine tumours. But surgery isn’t always possible. Some small bowel neuroendocrine tumours might have already started to spread when you are diagnosed. Or you might not be well enough to have it. You continue to have treatment to help your symptoms if surgery isn’t an option. Deciding which treatment you need A team of doctors and other professionals discuss the best treatment and care for you. They
Treatment by type of stomach NET
The treatment you have for a stomach neuroendocrine tumour (NET) depends on a number of things. This includes the type of NET and whether it has spread. Doctors call this the stage of the cancer. NETs grow at different rates, but they often grow very slowly. Some might not grow at all for months or years. So, you might not need treatment straight away. Your doctor might ask you to have regular tests to keep an eye on it. Which treatment do I need? A team of doctors and other professionals discuss the best treatment and care for you. They
Thymus gland cancer
Cancer of the thymus gland is rare. Most cancers that start in the thymus gland are called thymomas. There’s also a much rarer form of thymus gland cancer called thymic carcinoma. What is the thymus gland? The thymus gland is in your chest, in between your lungs. A gland is an organ in your body that makes and releases substances such as hormones. The thymus gland is part of our lymphatic system . It’s involved in the development of a type of white blood cell called a T lymphocyte. These white blood cells are part of your immune system .
Treating Wilms tumour
Doctors plan your child’s treatment in one of the UK’s children’s cancer centres. Your child has most of their treatment in this specialist centre, but some care might take place at a hospital closer to home. Children’s cancer centres have teams of specialists who know about Wilms tumours and the best way to treat them. Wilms tumour is curable in about 9 out of 10 children (about 90%). The main treatments include: chemotherapy for almost all children surgery for all children radiotherapy for some children In the UK and many other countries, children usually start treatment without having a biopsy if the tumour looks
Treating tonsil cancer
The main treatments for tonsil cancer are surgery, radiotherapy and chemotherapy. You might have a combination of these or one treatment on its own. The tonsils are part of the oropharynx and treatment is similar to other cancers of the oropharynx. Treatment by stage Staging is a way of describing the size of cancer and how far it has grown. We have information about treatment for early and advanced cancer. Your doctor will tell you more about the stage of your cancer and the treatment you will have. There is an increase in the number of tonsil cancers that are
Treating tongue cancer
The main treatments for tongue cancer are surgery, radiotherapy and chemotherapy, either combined or on their own. Your treatment depends on how big the cancer is and whether it has spread (the stage). It also depends on which part of the tongue is affected. Treating the oral tongue The front two thirds of the tongue (oral tongue) are treated like a mouth cancer. Early stage Early cancer means your cancer is smaller than 4cm and is contained within the tongue. The most common treatment is surgery to remove the affected area. You might also have radiotherapy after surgery to try
Placental site trophoblastic tumour and epithelioid trophoblastic tumour
Placental site trophoblastic tumours (PSTTs) and epithelioid trophoblastic tumours (ETTs) are cancers that happen after pregnancy. They are extremely rare and are slow growing. What are placental site trophoblastic tumours and epithelioid trophoblastic tumours? These tumours are part of a group of conditions called gestational trophoblastic disease (GTD). GTD is the name for abnormal cells or tumours that grow from the tissue that forms in the womb during pregnancy. Less than 1 in 100 (less than 1%) of GTDs are placental site trophoblastic tumours or epithelioid trophoblastic tumours. In PSTT and ETT the tumour develops from the cells that grow
Recovery package for cancer
The recovery package is a set of interventions that your healthcare team uses. An intervention means that you and your team find ways to help you with your care needs and worries as they come up. It helps to improve your experience of living with cancer. The recovery package aims to support people affected by cancer to: feel more in control improve their quality of life Your medical team at the hospital and GP work together to make sure you receive the recovery package. The recovery package is available throughout England. In Northern Ireland, Scotland and Wales, there are similar
How do I mentally prepare for cancer treatment?
You can help yourself to get ready for cancer treatment by looking after your mental wellbeing. Focussing on your mental health is one part of prehabilitation. This is a programme of advice and support that can help to prepare you for treatment. The other parts are eating a varied diet and being physically active. Focusing on these three areas, in whatever time you have before treatment starts, can help you: feel more in control of your health cope better during treatment recover better And by making it part of life with cancer, it can help you to live well in
How do I physically prepare for cancer treatment ?
You can help yourself to get ready for cancer treatment by being physically active. Being more active and exercising is one part of prehabilitation. This is a programme of advice and support that can help to prepare you for treatment. The other parts are eating a varied diet and looking after your mental wellbeing. Focusing on these three areas, in whatever time you have before treatment starts can: help you feel more in control of your health cope better during treatment recover better And by making it part of life with cancer, it can help you to live well in the
What should I eat to prepare for cancer treatment ?
You can help yourself to get ready for cancer treatment by trying to eat a wide range of foods in the right proportions, also called a varied diet. This includes eating enough protein, calories and other nutrients. Eating a varied diet is one part of prehabilitation. This is a programme of advice and support that can help to prepare you for treatment. The other parts are being physically active and looking after your mental wellbeing. Focusing on these three areas, in whatever time you have before treatment starts, can help you: feel more in control of your health cope better during
What is prehabilitation ?
Prehabilitation (prehab) means getting ready for cancer treatment in whatever time you have before it starts. It is a programme of support and advice that some NHS hospitals are using. It covers three particular parts of your health: what you’re eating and your weight physical activity or exercise mental wellbeing Stopping smoking and cutting down on alcohol can also help. It helps while you’re having treatment, with your recovery, as well as improving your overall health. How does prehabilitation help? At diagnosis, your medical team should screen you for any problems in the three areas above. Research shows that if you
X-rays
An x-ray is a test that uses small amounts (doses) of radiation to take pictures of the inside of your body. They are a good way to look at bones and can show changes caused by cancer or other medical conditions. X-rays can also show changes in other organs, such as the lungs. You usually have x-rays in the imaging department of the hospital, taken by a radiographer. But in an emergency they are sometimes done on the ward. Types There are different types of tests using x-rays, including: chest x-rays to show fluid, signs of infection, an enlarged heart or tumours in the chest
Womb biopsy
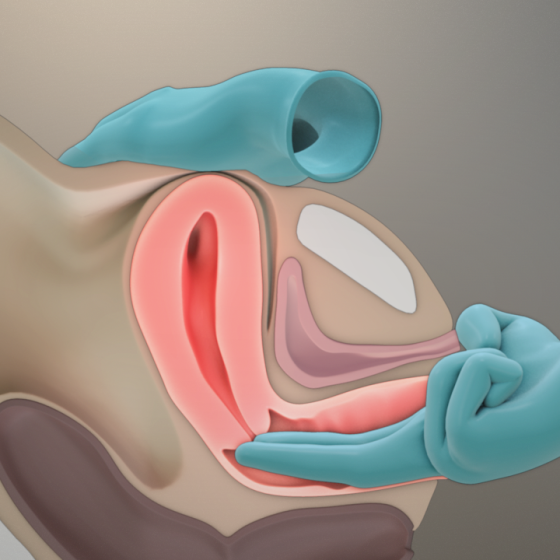
The only way to definitely diagnose womb cancer is to take a sample of the tissue lining the womb. This is called an endometrial biopsy. Your doctor sends the sample to the lab. This is where a pathologist checks it for abnormal or cancerous cells. There are different ways to take a biopsy of the womb lining. Aspiration biopsy To have this test you lie on your back on a couch with your knees up and feet apart. You’ll need to remove your underwear, but you will have a sheet to cover yourself with. Your doctor or nurse gently opens your vagina with a speculum. This is just the same as when
Vulval biopsy
A vulval biopsy means removing a sample of tissue from the vulva. This is the best way to find out whether or not you have vulval cancer or another vulval condition. Preparing for your vulval biopsy You usually have this test as a day patient using a local anaesthetic. Rarely, you may have it under a general anaesthetic. This is when you are asleep and don’t feel anything. Your doctor or nurse will ask you to sign a consent form once they have given you information about the test. Eating and drinking You usually have a vulval biopsy under local anaesthetic,
Video of your vocal cords (videostroboscopy)
This test uses a long, thin, flexible tube called an endoscope to examine your voice box (larynx) and vocal cords while you speak. The endoscope has a camera and light and is connected to a video monitor and recorder. It helps your doctor to see the movement of your vocal cords while you speak. This test is also called a videostroboscopy, or videolaryngoscopy with stroboscopy. Why do you have a videostroboscopy? You have a video of your vocal cords to help your doctor see how they move when you speak. It also gives your doctor a chance to look for abnormalities on
Video of your throat and larynx (transnasal oesophagoscopy)
In this test the doctor uses a long, flexible telescope through your nose. This is to make a video of the inside of your: nose throat voice box (larynx) upper part of the food pipe (oesophagus) The test is called a transnasal oesophagoscopy. Why do you have a transnasal oesophagoscopy? This test helps your doctor to view your voice box (larynx) and food pipe (oesophagus). You might have it instead of having an endoscopy. This might happen if you aren’t well enough to have a general anaesthetic. Endoscopy instruments are bigger. You usually need a general anaesthetic for an endoscopy. How to prepare for
Vaginal biopsy
Your doctor may want you to have a biopsy. This means removing a sample of tissue from the vagina. You might have this done during a colposcopy or as a separate test. The doctor sends the sample to the laboratory where a pathologist examines it. You might have: an excision biopsy a punch biopsy Why do you have this test? You have a vaginal biopsy to find out if you have pre cancerous changes (VAIN) or cancer of the vagina. If you have cancer, looking at the cells under a microscope will show which type of vaginal cancer it is. Your doctor may
Ultrasound scan of the ovaries
Ultrasound scans use high frequency sound waves to create a picture of a part of the body. It can show the ovaries, womb and surrounding structures. You might have this test to help diagnose ovarian cancer. To have an ultrasound scan of the ovaries, your doctor or radiographer moves a probe over the lower part of your tummy. You may also have an internal vaginal ultrasound. This is when your doctor gently puts the probe into your vagina. This is also called a transvaginal ultrasound scan. We have separate information about what happens during a transvaginal ultrasound scan. Why you have it
Ultrasound scan
An ultrasound scan is a procedure that uses high frequency sound waves to create a picture of a part of the inside of your body. The ultrasound scanner has a probe that gives off sound waves. The probe looks a bit like a microphone. The sound waves bounce off the organs inside your body, and the probe picks them up. The probe links to a computer that turns the sound waves into a picture on the screen. Ultrasound scans aren’t painful but can cause some discomfort. You might have it at one of the following: your GP surgery local community clinic in your
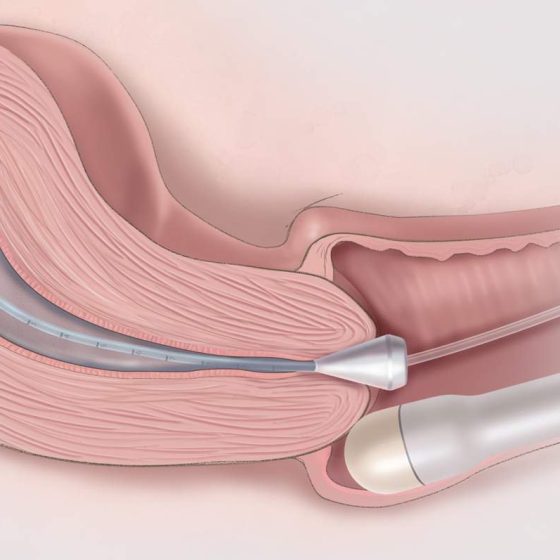
Transvaginal ultrasound scan
An ultrasound scan is a procedure that uses high frequency sound waves to create a picture of a part of the inside of your body. The ultrasound scanner has a probe that gives off sound waves. The probe looks a bit like a microphone. The sound waves bounce off the organs inside your body, and the probe picks them up. The probe links to a computer that turns the sound waves into a picture on the screen. Ultrasound scans aren’t painful but can cause some discomfort. You might have it at one of the following: your GP surgery local community clinic in your
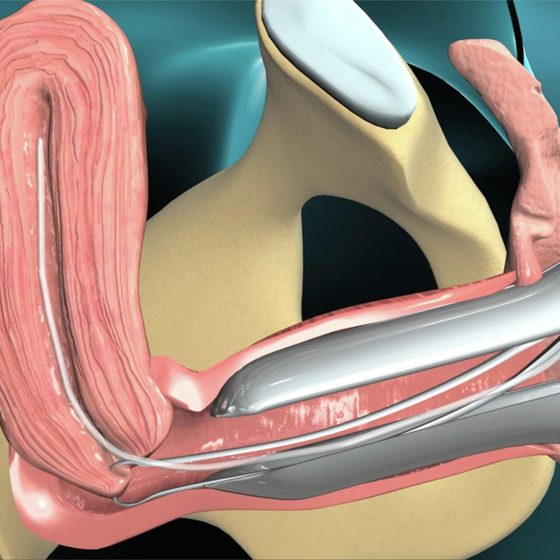
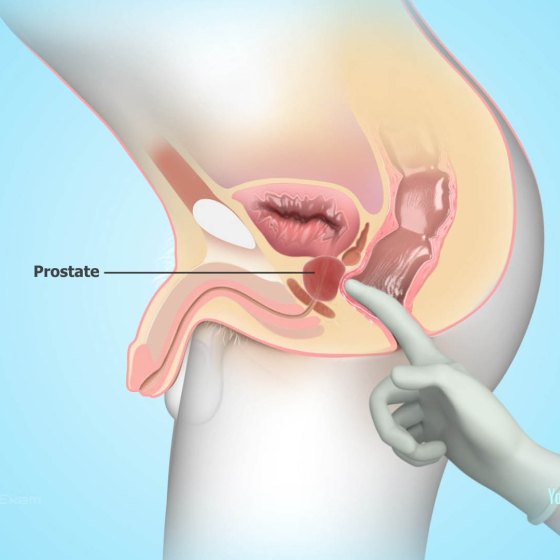
Transrectal ultrasound scan (TRUS) and biopsy for prostate cancer
A transrectal ultrasound scan (TRUS) is an examination of the prostate gland using ultrasound. Your doctor might take samples of tissue from the prostate during this test. This is a TRUS guided biopsy. It can help to diagnose prostate cancer. You usually have an MRI scan before your TRUS guided biopsy. The MRI scan helps your doctor decide whether you need a biopsy and where to take the biopsies from. What is a TRUS? Ultrasound scans use high frequency sound waves to create a picture of a part of the body. A prostate ultrasound scan can show changes in your
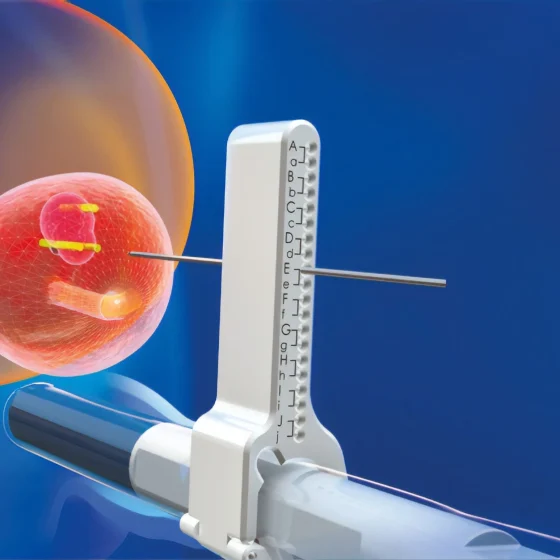
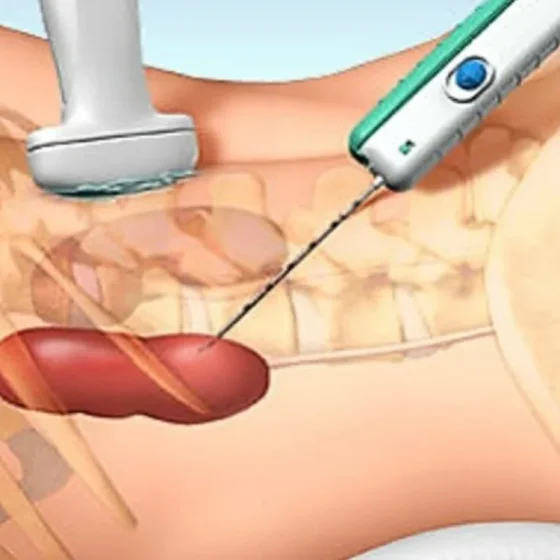
Transperineal biopsy for prostate cancer
A transperineal biopsy is a needle biopsy to look for cancer cells in the prostate. This helps to diagnose prostate cancer. Your doctor puts a needle into the prostate through the skin behind the testicles (perineum). They take a number of samples, which are sent to the laboratory. In the laboratory, a specialist doctor looks at the samples under the microscope. Preparing for your transperineal biopsy You usually have this test in the outpatient department under local anaesthetic. Sometimes, you may have it in the operating theatre under a general anaesthetic. This is when you are asleep and don’t feel anything. Your doctor
Tissue typing
Tissue typing is a set of tests that are done with your blood and saliva. You might have it if your doctors think that you need a stem cell or bone marrow transplant from someone else (donor transplant). It is to show how closely a possible stem cell or bone marrow donor’s tissue matches your own. You might also hear this test called other names such as: HLA tissue typing HLA typing Histocompatibility testing HLA crossmatching You usually have one or more of the following tests: a blood test a swab taken from the inside of your cheek (buccal swab)
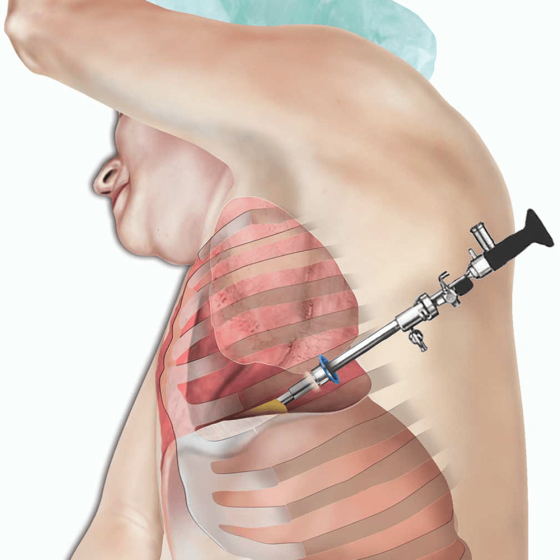
Thoracoscopy and pleural biopsy
Thoracoscopy is a test to look at the space between your lung and chest wall. This is the pleural cavity. You might have a thoracoscopy to check for signs of cancer such as mesothelioma. It is a small operation. The doctor uses a flexible tube with a light and video camera attached. This is called a thoracoscope. They use it to take samples (biopsies) from the tissues that cover your lung (pleura). Why you might have it You have a thoracoscopy to look inside your chest to see possible areas of cancer. Doctors use a thoracoscopy to help diagnose cancers
Surgical biopsy for lung cancer
During a surgical biopsy for lung cancer, your surgeon takes a sample of the lung tissue by making small cuts in your chest. The surgeon carries out your biopsy in one of the following ways: keyhole surgery , also called video assisted thoracoscopy surgery (VATS) open surgery, through a small cut in the chest wall (small thoracotomy) You have this test under general anaesthetic . So, you will be asleep and won’t feel anything. Why do I need a surgical biopsy? A surgical biopsy of the lung can help diagnose lung cancer. You might have this test if: a CT
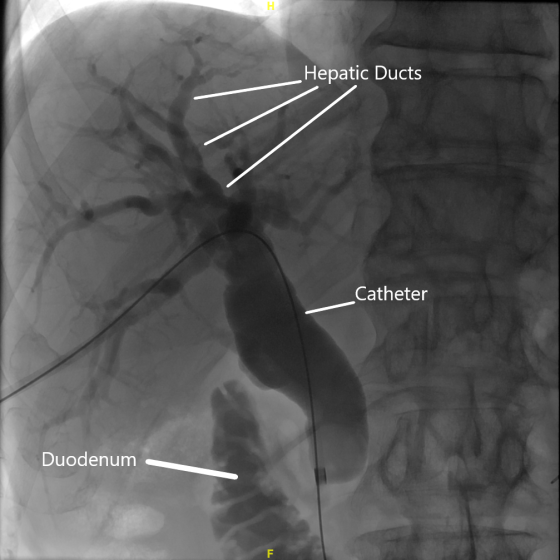
Percutaneous transhepatic cholangiography (PTC)
A percutaneous transhepatic cholangiography (per-kew-tay-nee-us trans-hep-attic col-an-jee-og-raf-ee) is a way of looking at your bile ducts using x-rays. This test is also called PTC. Your doctor puts a long thin needle through the skin and into your liver and bile ducts. They take x-rays of the pancreas, gallbladder and bile ducts. They can also take samples (biopsies) of any abnormal looking areas. You usually have a PTC if you can’t have an ERCP for any reason or if you have had an ERCP but it didn’t work. For example, if doctors weren’t able to take samples of tissue or drain the bile ducts. Why
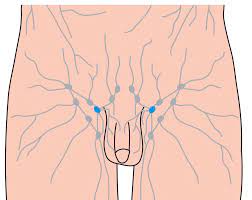
Penile dynamic sentinel lymph node biopsy
A dynamic sentinel lymph node biopsy (DSLNB) is a test to find out if there is cancer in the lymph nodes near your cancer. Not everyone with penile cancer needs a sentinel lymph node biopsy. You might have this test if there is no obvious sign that cancer cells have spread to the lymph nodes after: you have been examined by your specialist you have had an ultrasound scan It means that your doctor can avoid removing all the lymph nodes in the groin if this is not necessary. You may have to travel to a specialist hospital for this test. This is
Pelvic examination under anaesthetic
This is an internal examination under general anaesthetic . An examination under general anaesthetic is also called an EUA. The examination includes checking your: cervix, vagina and vulva womb bladder anus and rectum (back passage) Your doctor (gynaecological oncologist) can take samples of tissue (biopsies) during the test if necessary. Why you might have a pelvic examination under anaesthetic You might have this examination to check for signs of cancer. It can help your doctor diagnose a number of cancers such as: Preparing for a pelvic examination under anaesthetic Your doctor checks that you are fit and well enough for a general anaesthetic. Let
Pelvic examination
A pelvic examination is when a doctor or a specialist nurse examines your pelvis. Your pelvis is the area between your hip bones. It contains the pelvic organs, including the: bladder lower part of the bowel In women, it also contains the female reproductive system . This includes the: ovaries fallopian tubes womb cervix vagina You may also hear your doctor calling this test an internal or vaginal examination. During the pelvic examination, your doctor looks and feels for anything that doesn’t feel normal. They might refer you for more tests or treatment if they find anything abnormal. Your doctor
Panendoscopy
A panendoscopy is a test to look at your upper airway. This includes your: mouth nose throat voice box top of your food pipe A specialist doctor does the test using a panendoscope, which is a series of connected telescopes. They look through one end and there is a camera and light at the other. Why you have it You might have a panendoscopy to: get a more detailed look at an abnormal area take tissue samples from an abnormal area (a biopsy) This is a common test if you have symptoms that could be due to head and neck cancer. Before your test You
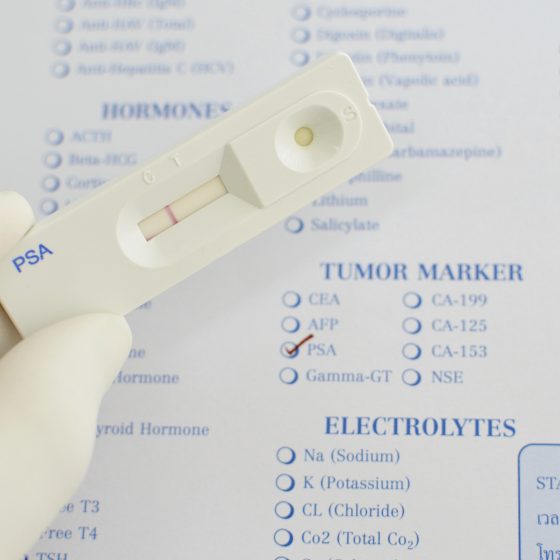
PSA test
The PSA test is a blood test that measures the amount of prostate specific antigen (PSA) in your blood. It can help to diagnose prostate cancer. Your doctor or nurse takes a sample of your blood. This can be done at your GP practice. They then send this off to a laboratory to check the amount of PSA. When you have the test You might have a PSA test if you: have symptoms that could be caused by prostate cancer are aged 50 and over and have asked your GP for a test Doctors also check your PSA level as you
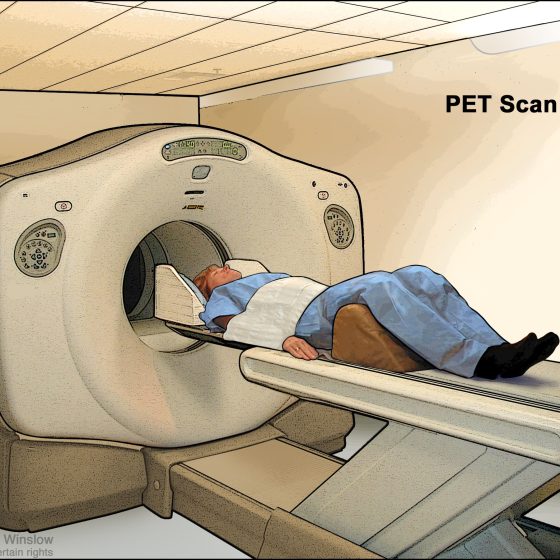
PET-MRI scan
A PET-MRI scan combines a PET scan and an MRI scan into one to give detailed information about your cancer. PET stands for positron emission tomography. It uses a mildly radioactive liquid (radioactive tracer) to show up areas of your body where cells are more active than normal. MRI stands for magnetic resonance imaging. It uses magnetism and radio waves to create cross section pictures of the body. It shows up soft tissues very clearly. You usually have a PET-MRI scan in the nuclear medicine or radiology department as an outpatient. These scanners tend to be only in the major
PET-CT scan
A PET-CT scan combines a CT scan and a PET scan. It gives detailed information about your cancer. The CT scan takes a series of x-rays from all around your body and puts them together to create a 3 dimensional (3D) picture. The PET scan uses a mildly radioactive liquid (radioactive tracer) to show up areas of your body where cells are more active than normal. You usually have a PET-CT scan in the radiology department as an outpatient. A radiographer operates the scanner. It usually takes between 30 and 60 minutes. These scanners tend to be available only in the major cancer hospitals. So you
PET scan
A PET scan is a test that creates 3 dimensional (3D) pictures of the inside of your body. PET stands for positron emission tomography. The PET scan uses a mildly radioactive liquid (radioactive tracer) to show up areas of your body where cells are more active than normal. It’s used to help diagnose some conditions, including cancer. It can also help to find out where and whether cancer has spread. You usually have a PET scan in the radiology or nuclear medicine department as an outpatient. These scanners tend to be only in the major cancer hospitals. So you might have to
Neuroendoscopy to take a sample of tissue
Neuroendoscopy is a way of taking samples of tissue from a brain tumour. Doctors take samples of tissue (biopsy) to look at it under a microscope. This helps your doctor decide the best treatment for you. You may also have a neuroendoscopy to: remove fluid from the fluid filled spaces of the brain (ventricles) remove all or part of the brain tumour You usually have a neuroendoscopy under general anaesthetic. This means that you will be asleep and won’t feel anything. Having a neuroendoscopy sounds like a frightening procedure, but it is quite safe. Doctors who carry out these procedures
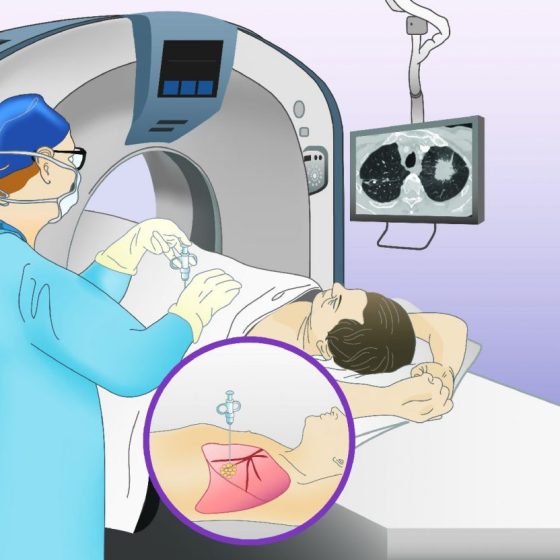
Needle biopsy through the skin for lung cancer
This test is also called a percutaneous lung biopsy. A doctor called a radiologist takes a sample of lung tissue by passing a needle into the lung. They use a CT scanner or ultrasound to ensure they know the right place to take the sample. You have this test with a local anaesthetic . It takes about 30 to 45 minutes. Why do I need a biopsy through the skin? You might have this test if your doctor has seen an abnormal looking area in your lung or airways using an x-ray or CT scan. What do I need to
Needle biopsy of the thyroid
You have this test to find out if the lump in your thyroid needs further treatment. Preparing for your test You are able to eat and drink normally before a biopsy. Take your medicines as normal. But if you are taking any blood thinning medicines you might need to stop them before the test. Your doctor or nurse will tell you when to stop. You will need to remove any clothing around your neck such as a tie or scarf. You will also be asked to remove any jewellery such as a necklace or chain. You will lie on your back on a
Neck lymph node ultrasound and biopsy
During a neck lymph node biopsy, your doctor uses an ultrasound scanner to help them take a small amount of lymph node tissue using a fine needle. Ultrasound scans use high frequency sound waves to create a picture of a part of the body. The ultrasound scanner has a probe that gives off sound waves. The sound waves bounce off the structures inside your body, and the probe picks them up. The probe links to a computer that turns the sound waves into a picture. You normally have this test as an outpatient procedure in the hospital’s imaging department. Why
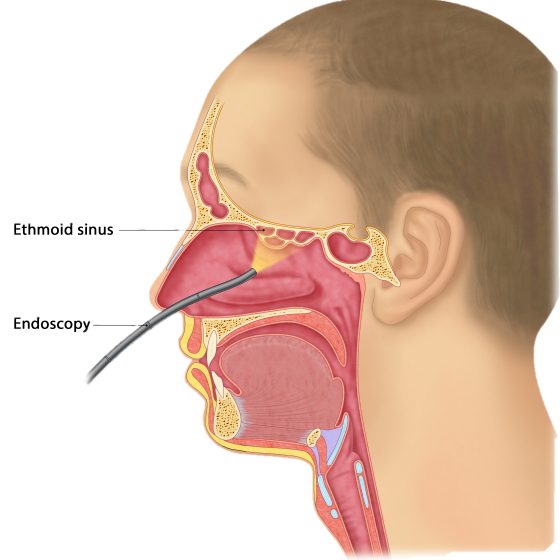
Nasoendoscopy
A nasoendoscopy is part of a normal ear, nose and throat examination. It is a procedure to look at the inside of the: nose back of the tongue throat voice box Your doctor passes a thin rigid or flexible tube called a nasoendoscope through your nostril into your nose. The tube has a camera and a bright light at the end. Why you might have it You may have a nasoendoscopy so that your doctor can check for any abnormal looking areas. This is a common test if you have symptoms that could be due to head and neck cancer. Preparing for
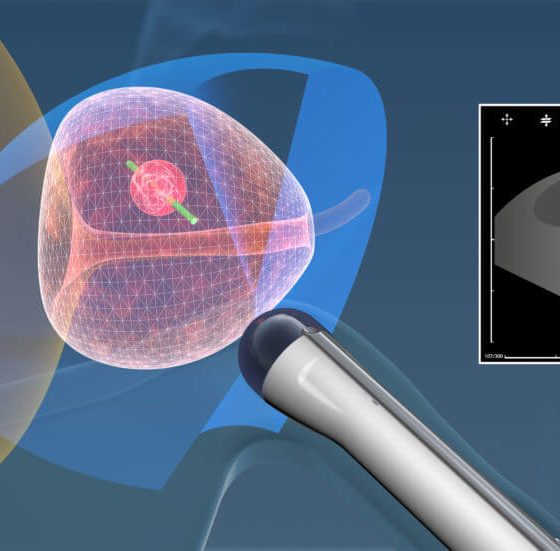
Multiparametric MRI (mpMRI) scan for prostate cancer
MRI stands for magnetic resonance imaging. It is a type of scan that creates pictures using magnetism and radio waves. MRI scans produce pictures from angles all around the body and shows up soft tissues very clearly. The multiparametric MRI (mpMRI) is a special type of MRI scan that produces a more detailed picture of your prostate gland than a standard MRI scan does. You usually have an mpMRI scan if doctors suspect that you have prostate cancer. Why you might have an mpMRI It is important to know that an mpMRI scan alone cannot diagnose prostate cancer. But it can
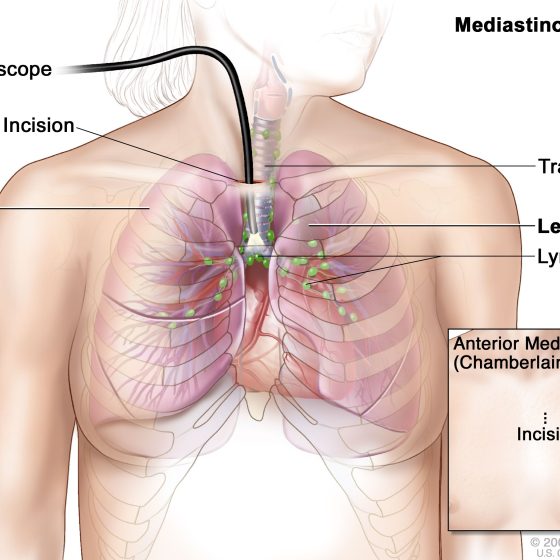
Mediastinoscopy
Mediastinoscopy is a test that examines the mediastinum. This is the centre of your chest and area between your lungs. It contains: the heart the main blood vessels lymph nodes (glands) the food pipe (oesophagus) The mediastinoscopy takes between 45 to 60 minutes. You have a general anaesthetic to have this test. Why do I need a mediastinoscopy? You might have this test to see if cancer cells have spread into the lymph nodes around the windpipe. Preparing for your mediastinoscopy You see a doctor before the mediastinoscopy. They’ll ask some general questions about your health. You will also need some other tests before
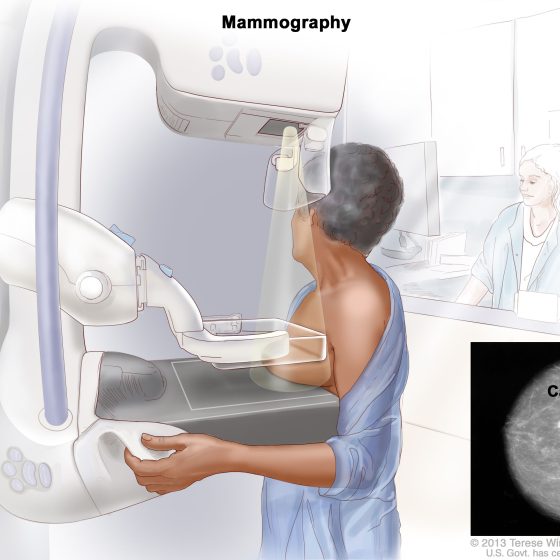
Mammogram
A mammogram is an x-ray of your breasts. X-rays use high energy rays to take pictures of the inside of your body. You might have mammograms: as part of the breast cancer screening programme to check for cancer if you have symptoms that could be due to breast cancer. This is called a diagnostic mammogram The health professionals who take mammograms are called mammographers. The mammogram itself usually only takes a few minutes, but the appointment may last about 30 minutes. Mammograms for breast screening Mammograms for breast screening can help to find breast cancer early when they are too
MRI scan
MRI (magnetic resonance imaging) is a type of scan that uses magnetism and radio waves to take pictures of inside the body. The scan takes between 15 and 90 minutes. You might have one to find out whether you have cancer and if you do to measure how big it is and whether it has spread. You might also have one to see how well treatment is working. It is a safe test. If you have an injection of contrast dye it can cause a headache, dizziness or a warm flushed feeling An MRI is a type of scan that creates
MRCP and MRI scan
MRCP stands for magnetic resonance cholangio pancreatography (col-an-jee-oh pan-kree-at-og-raf-ee). An MRCP scan is a type of MRI scan that you have in an MRI scanner. MRI stands for magnetic resonance imaging. An MRI scan produces pictures from angles all around the body and shows up soft tissues very clearly. These scans create pictures using magnetism and radio waves to give detailed pictures of your: pancreas gallbladder bile ducts liver You might have an MRI scan of your tummy (abdomen) at the same time as the MRCP. You usually have these scans in the x-ray (radiology) department as an outpatient. It can
Radioactive scans for neuroendocrine tumours (NETs)
Radioactive scans can help your doctors diagnose some types of neuroendocrine tumours. You have an injection of a low dose radioactive substance, which can show up on a scan. Radioactive scans include: octreotide scans (or Octreoscans) – these are also called somatostatin receptor scintigraphy scans tektroyd scans gallium dotatate PET (positron emission tomography) scans You might also have an mIBG scan, but this is less common now. mIBG stands for metaiodobenzylguanidine. What are radioactive scans and why do I need one? Octreotide, dotatate and mIBG are substances that some neuroendocrine cells take up (absorb). Doctors can attach a radioactive substance
Lymph node ultrasound and biopsy – under the arm (axillary)
Cancer can sometimes spread into the lymph nodes under the arm (axilla). This can happen with different types of cancer, including breast cancer. To check the lymph nodes under your arm for breast cancer cells, you have an ultrasound scan. Ultrasound scans use high frequency sound waves to create a picture of a part of the body. The ultrasound scanner has a microphone that gives off sound waves. The sound waves bounce off the organs inside your body and are picked up by the microphone. The microphone links to a computer and turns the sound waves into a picture. If
Lymph node ultrasound and biopsy – groin
Cancer can sometimes spread into the lymph nodes in the groin. Your groin is the area at the top of your legs, between the hips. This can happen with different types of cancer, such as anal and penile cancer. To check the lymph nodes in your groin for cancer cells, your doctor checks the groin for swollen (enlarged) lymph nodes. You then might have an ultrasound scan to check the nodes. Ultrasound scans use high frequency sound waves to create a picture of a part of the body. If doctors find any abnormal lymph nodes, they use the ultrasound to
Lumbar puncture
A lumbar puncture is a test to check the fluid that circulates around the brain and spinal cord. This is called the cerebrospinal fluid or CSF. Why do I need a lumbar puncture? A lumbar puncture can check for cancer cells or for infection in the CSF. Doctors remove some of the CSF to test for cancer cells. They use a needle to take a sample of the CSF from your lower back. You normally have this test in the outpatient department under local anaesthetic. This means you are awake but the area is numb. What Is a Lumbar puncture? A
Liver biopsy
A biopsy means removing a sample of cells or tissue and looking at it under a microscope. You may have a liver biopsy to help diagnose liver cancer. But not everyone needs to have a liver biopsy. Doctors can often diagnose liver cancer just by looking at the scans. You usually won’t have a liver biopsy if your doctor thinks: they can remove the cancer you may be able to have a liver transplant This is because there is a small risk that a liver biopsy could spread the cancer along the path of the biopsy needle. It is important to
Laryngoscopy
A laryngoscopy is a test that an ear, nose and throat (ENT) specialist uses to look at the: back of your throat (pharynx) voice box (larynx) The ENT specialist uses a thin tube called a laryngoscope to do this test. They can see the inside of your throat very clearly. You have this test under general anaesthetic. This means that you are asleep and won’t feel anything. Your doctor might also call this test an examination under anaesthesia (EUA). They may take samples of tissue (biopsy) of any abnormal areas. Preparing for a laryngoscopy You might have a blood test 2 days beforehand to check
Laparoscopy
Laparoscopy is a small operation to look inside your tummy (abdomen) and the area between your hips (pelvis). Laparoscopy is also known as keyhole surgery or minimally invasive surgery. It can help diagnose certain types of cancer. It is also a very common procedure used to treat and diagnose many other non cancerous conditions. A laparoscopy involves your surgeon making several small cuts (incisions) instead of a large incision across your abdomen. The surgeon places hollow tubes inside the incisions. These are called ports. Your surgeon puts a thin tube with a light and a camera (laparoscope) through one of
LLETZ – Large Loop Excision of the Transformation Zone
LLETZ stands for large loop excision of the transformation zone. It’s also known as loop electrosurgical excision (LEEP) or loop diathermy. Your colposcopist uses a thin wire loop to remove the transformation zone of the cervix. The wire has an electrical current running through it, which cuts the tissue and seals the wound at the same time. The transformation zone is the area around the opening of the cervix. LLETZ is an outpatient treatment and takes up to 15 minutes. You usually have it under local anaesthetic. Why you might have LLETZ LLETZ is a treatment for abnormal cervical cells picked
Kidney biopsy
A kidney biopsy is a procedure to take a small piece of tissue from the kidney. A specialist doctor (pathologist) looks at it under a microscope and can tell if you have kidney cancer and which type it is. Knowing this helps your doctor decide on the best treatment for you. Why you might have a kidney biopsy Your doctor will ask you to have a kidney biopsy to: find out if you have kidney cancer if other tests haven’t been clear help them decide if a small kidney cancer can be watched before being treated (active surveillance) tell them
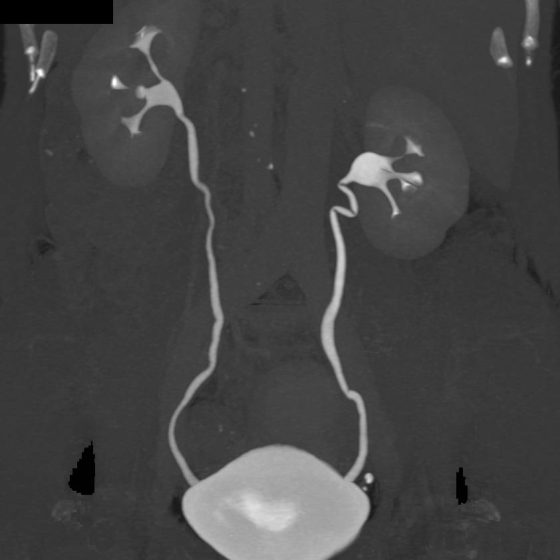
IVU (Intravenous urogram) or IVP (Intravenous pyelogram)
An intravenous urogram (IVU) is a test that looks at the whole of your urinary system. It’s sometimes called an intravenous pyelogram (IVP). It looks at the: kidneys bladder tubes that connect the kidney with the bladder (ureters) The male urinary system The female urinary system The test uses a colourless dye, also called contrast medium. This shows up the soft tissues of the urinary system on a normal x-ray. Why do I need an IVU test? An IVU test can show if cancer is growing in any part of your urinary system. The cancer will show up as a
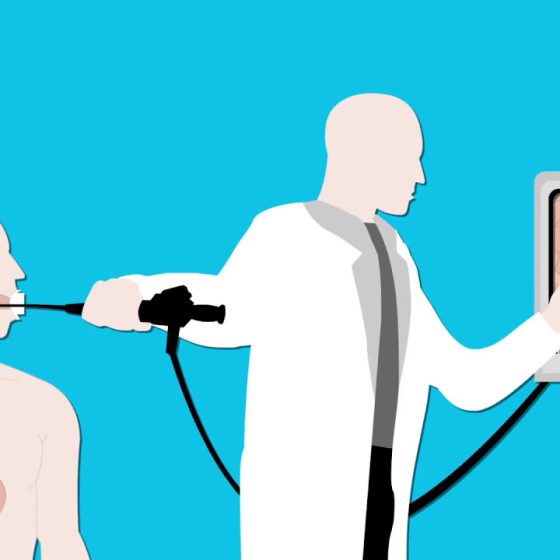
Gastroscopy for stomach cancers
A gastroscopy is a test that looks at the inside of your food pipe (oesophagus), stomach and the first part of your small intestine (small bowel). A doctor or specialist nurse (endoscopist) does the test. They use a long flexible tube which has a tiny camera and light at the end. This tube is called a gastroscope or endoscope. You may also hear this test called an endoscopy or oesophago gastric duodenoscopy (OGD). Why do I need a gastroscopy? You might have a gastroscopy to find out the cause of symptoms such as: abnormal bleeding indigestion or heartburn that doesn’t go away with
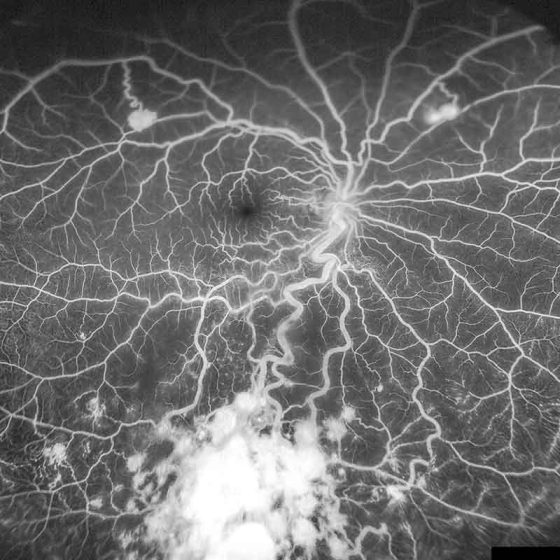
Fluorescein angiogram of the eye
Your eye specialist might do a fluorescein angiogram (FA) to look at the blood vessels in your eye. You may also have a photograph taken of the surface of the inside of the eye (the fundus). Doctors call this colour fundus photography. What is it? A fluorescein angiogram looks at the blood vessels and the lining at the back of your eye (the retina). This test can pick up changes in the condition of your eyes. It can help your specialist make a diagnosis of eye cancer or tell them how well treatment is working. What happens You usually have the test in the
Flexible sigmoidoscopy
Flexible sigmoidoscopy is a test to look inside the lower part of your large bowel. It is also called bowel scope or flexi sig. The flexible sigmoidoscopy is a thin flexible tube called a colonoscope. This has a small light and camera at one end. The endoscopist (specially trained doctor or nurse) puts the tube into your back passage (anus). They then gently move it up into the lower part of your bowel. They can see the pictures of the inside of your bowel on a TV screen. You usually have this test in the endoscopy unit at the hospital. It may
FIT (Faecal Immunochemical Test)
FIT (Faecal Immunochemical Test) is a test that looks for blood in a sample of your poo. It looks for tiny traces of blood that you might not be able to see and which could be a sign of cancer. Traces of blood in your poo can be caused by other medical conditions and doesn’t necessarily mean you have cancer. But if it is cancer, finding it at an early stage means treatment is more likely to work. This information is about using the FIT test for people who have symptoms that could be caused by bowel cancer. We have separate
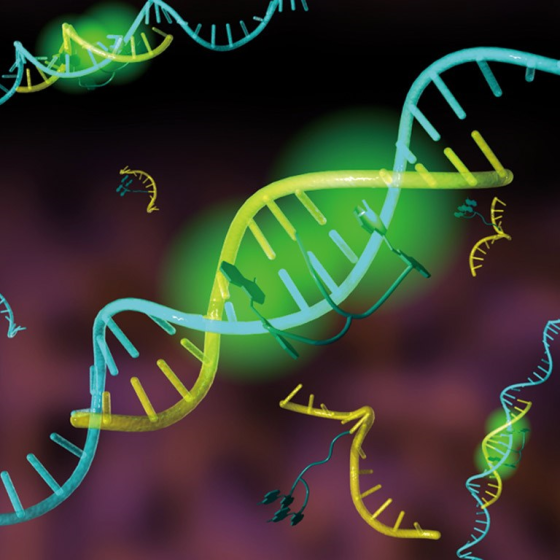
FISH (fluorescence in situ hybridisation)
FISH stands for fluorescence in situ hybridisation. It is a test that looks for gene changes in cells. Genes are made of DNA. They control everything the cell does, including when it grows and reproduces. FISH tests look for specific genes or parts of genes. Changes in genes can make the cancer cell: produce particular proteins make far more of the protein than normal stop making a particular protein If a gene change occurs, the cell may produce too much of a protein or not enough. This can make the cancer cells grow and reproduce more than normal. Cancer treatment There are now
Eye examination
The specialist eye doctor (ophthalmologist) will examine your eyes using a few different instruments. They look at the different structures of your eye to check for changes or abnormalities. What happens before the eye examination? You usually have drops into your eyes before the examination. These enlarge the pupils to make it easier for the eye specialist to look in your eyes. The eye drops might sting a bit when they first go in. They can cause blurred vision, and your eyesight may be blurry for a few hours, so you shouldn’t drive yourself home. It might be helpful to take
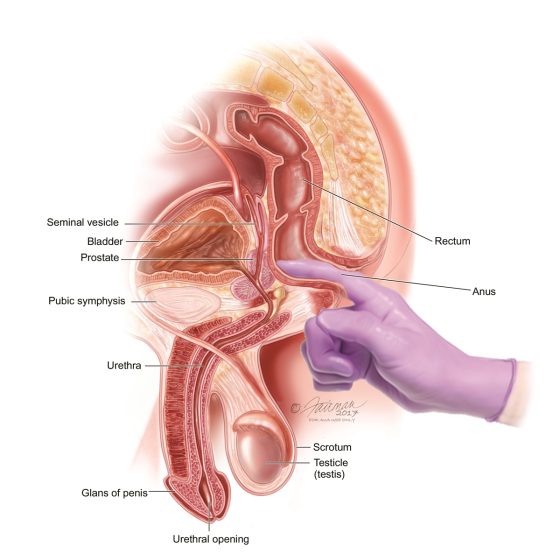
Examination of your prostate
To examine your prostate your doctor puts a finger into your back passage (rectum). This procedure is also called a digital rectal exam (DRE). Why you might have this You might have a prostate examination to check for any problems in your prostate. What happens before the examination? It’s normal to feel anxious about this test but it usually only takes a few minutes. You shouldn’t feel any pain but may be uncomfortable. Tell your doctor if you feel pain. You can ask for a man or woman doctor if you’d prefer. Or you can have someone else in the room,
Examination of anus and rectum (back passage)
This examination involves your doctor feeling inside the anus and rectum using their finger. This is also called a digital rectal exam (DRE). You might have a DRE if you have symptoms that could be due to bowel or anal cancer. Why you might have an examination of the anus and rectum You might have this to help work out the cause of your symptoms. Preparing for the examination It’s normal to feel anxious about this test but it usually only takes a few minutes. It might be uncomfortable but you shouldn’t feel any pain. Tell your doctor if you
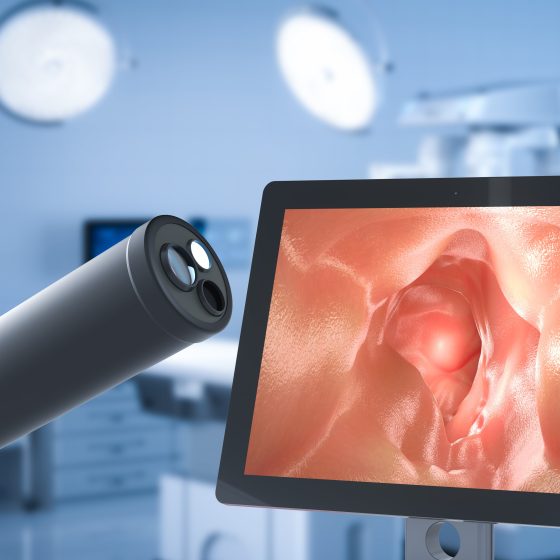
Endoscopy for cancers
An endoscopy is a test that looks inside the body. The endoscope is a long flexible tube which has a tiny camera and light on the end of it. There are many types of endoscopes and the doctor uses these to look inside different parts of the body. The name of the test you have will depend on which part of the body the doctor is looking at. Why do I need an endoscopy? You might have an endoscopy to help find out what is causing your symptoms. During this test a doctor or specialist nurse (endoscopist) can also take
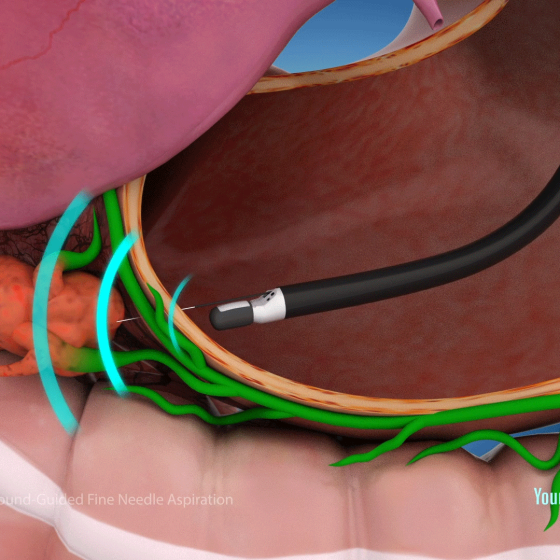
Endoscopic ultrasound for lung cancers
This test combines ultrasound and endoscopy. It helps your doctor to look through the wall of the food pipe at the surrounding tissue. The main airway (windpipe) is close to the food pipe. A doctor or a specialist nurse (endoscopist) does the test. To do the test the endoscopist uses a long flexible tube called an endoscope. They pass the endoscope down your throat into your food pipe. It has a tiny camera and light on the end and an ultrasound probe attached. The ultrasound scan uses high frequency sound waves to create a picture of the inside of your body. The
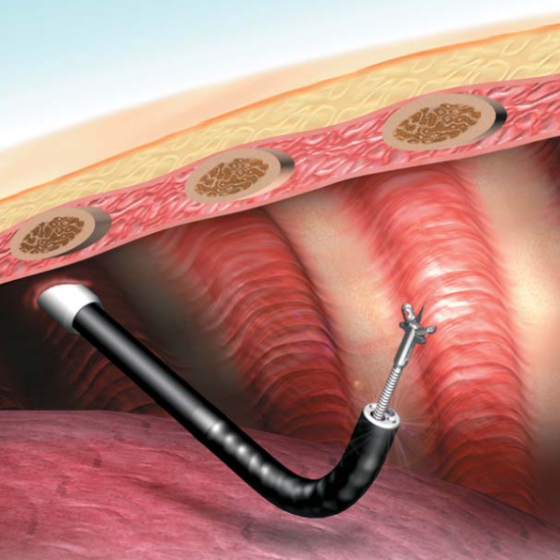
Endoscopic ultrasound (EUS)
This test combines an ultrasound and endoscopy. It can look at parts of your upper gastrointestinal tract. This includes the: food pipe (oesophagus) stomach pancreas bile ducts gall bladder first part of your small bowel (duodenum) lymph nodes An endoscopy is a test to look inside your body. Your doctor uses a long flexible tube (endoscope) with a tiny camera and light on the end. The endoscope also has an ultrasound probe at its tip. An ultrasound scan uses high frequency sound waves to create a picture of the inside of your body. The preparations for this test are the
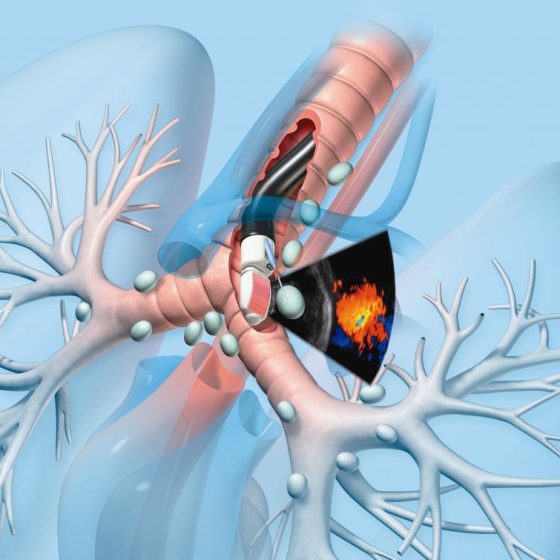
Endobronchial ultrasound (EBUS)
Endobronchial ultrasound is also called Endobronchial Ultrasound-guided Transbronchial Needle Aspiration (EBUS-TBNA). It is a test that can show if: an abnormal looking area is cancer the size of the cancer the cancer has spread into other lung areas or outside the lung This test uses a narrow flexible tube to look at the inside of the breathing tubes (airways) in your lungs. The tube has an ultrasound probe. It uses high frequency sound waves to create pictures of the lungs and structures outside the airway walls, such as the lymph nodes. Your doctor can see any areas that look abnormal
Echo (echocardiogram)
An echo is an ultrasound scan of the heart. This scan is very similar to the scans women have during pregnancy. It uses high frequency sound waves to create a picture of your heart. Doctors can look at the structure of your heart and how well it is pumping, and the nearby blood vessels. The ultrasound scanner has a microphone that gives off sound waves. The sound waves bounce off the heart and the microphone picks them up. The microphone links to a computer that turns the sound waves into a picture on the screen. This microphone device is called the probe.
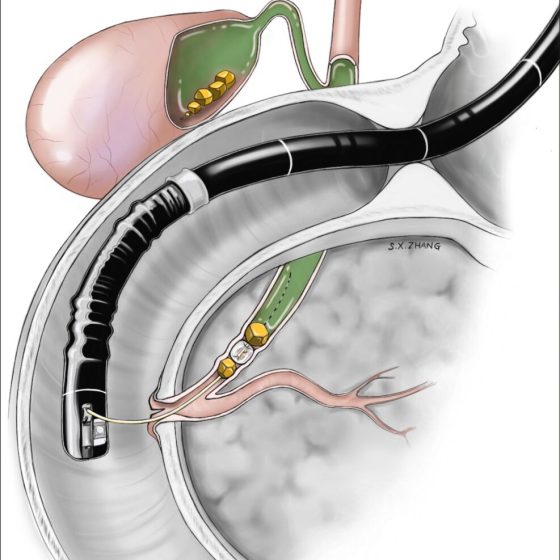
ERCP (endoscopic retrograde cholangiopancreatography)
ERCP test ERCP stands for endoscopic retrograde cholangio pancreatography. It is a test to help diagnose conditions of the liver, bile ducts, pancreas or gallbladder. What is an ERCP? Your doctor uses a long flexible tube with a small camera and light at the end, called an endoscope. It’s also sometimes called a duodenoscope. They pass this tube through your mouth, throat, stomach and into the first part of your small bowel (duodenum). Your doctor can look down the endoscope or see pictures on an X-ray screen of the pancreas, gallbladder and bile ducts. They can take samples (biopsies) of any abnormal looking areas.
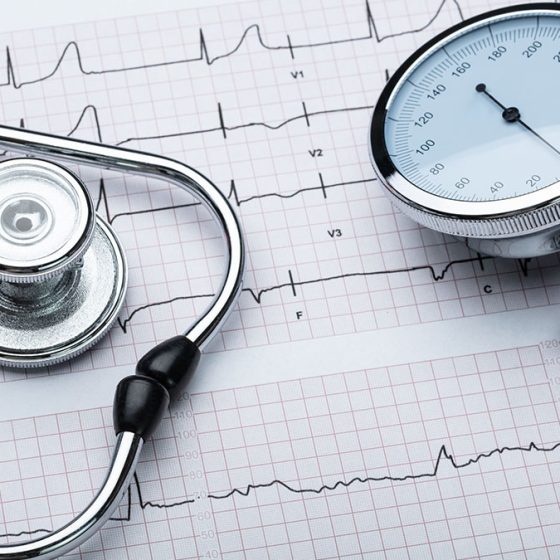
ECG (electrocardiogram)
An ECG is a test to check the electrical activity of your heart. It can show changes to your heart rate or rhythm and tell your doctor how well your heart is working. ECG stands for electrocardiogram. You might also hear this test called a heart trace. An ECG can give your doctor a lot of good information. It can help the doctor decide if you need further tests. To have the test a trained health care professional puts small sticky pads on your chest, arms and legs. Wires connect these to an ECG recording machine; these wires are ECG leads.
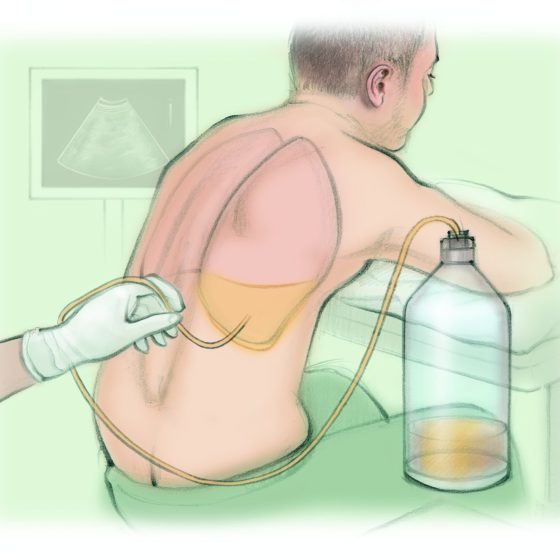
Draining fluid from your chest or tummy
Cancer cells can inflame the lung lining (pleura) or abdominal lining (peritoneum). This can cause fluid to build up. The fluid might contain cancer cells. Fluid around the lungs is called a pleural effusion. It can make it difficult to breathe. Draining fluid from your chest is called thoracocentesis or pleural aspiration. Fluid in the tummy (abdomen) is called peritoneal ascites. It can make the abdomen feel swollen, tight and uncomfortable. Draining fluid from your abdomen is called an abdoparacentesis or peritoneal aspiration. Why you might have it The doctors might drain fluid from around your lungs or abdomen to: see if the fluid contains
Looking at your mole or skin (dermoscopy)
You will see a skin specialist (dermatologist). They will ask you questions about your mole or abnormal area of skin, such as how long you have had it and what changes you have noticed. They will look closely at the abnormal area, and will check the rest of your skin for any changes. They usually use a dermatoscope to do this. What is a dermatoscope? A dermatoscope is a handheld instrument, a bit like a magnifying glass. It can make things bigger (magnify) by up to 10 times. Your specialist puts some oil or gel onto your skin. They then hold the dermatoscope
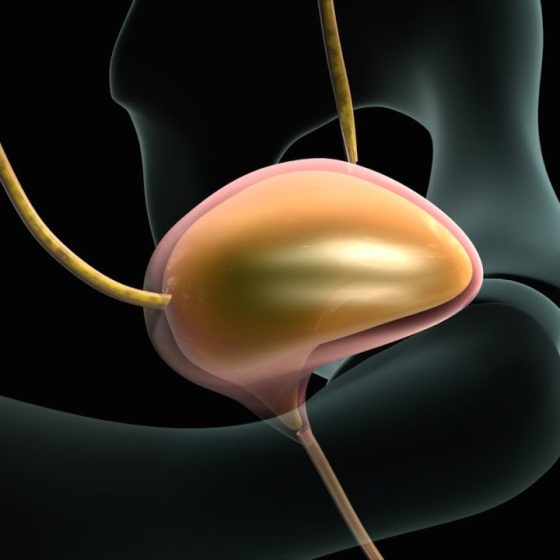
Cystoscopy to check for cancer
A cystoscopy is a test to look at the inside of your bladder and tube that carries urine from your bladder out of your body (urethra). It uses a thin tube called a cystoscope. There are different types of cystoscopies: flexible cystoscopy rigid cystoscopy narrow band imaging (NBI), blue light cystoscopy or photodynamic diagnosis (PDD) Your doctor will discuss with you what type of cystoscopy you’re having. Flexible cystoscopy The flexible cystoscope has optic fibres inside it, a light and camera attached to it. Because it’s flexible it can bend around the tubes as it passes through your urethra. This is generally done under local
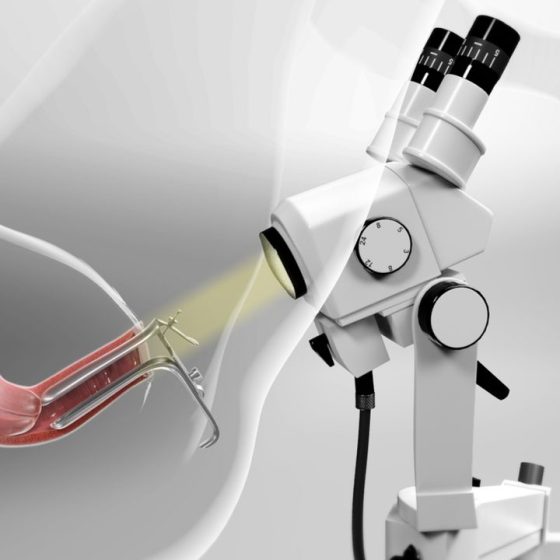
Colposcopy
A colposcopy is a test to look at the cervix in detail. A colposcope is a large magnifying glass that a doctor or specialist nurse (a colposcopist) uses to look closely at the skin-like covering of the cervix. By looking through it, the colposcopist can see changes that may be too small to see with the naked eye. They can take samples (biopsies) of any abnormal areas. You usually have a colposcopy in the hospital outpatient clinic. Why you might have a colposcopy You have a colposcopy if you’ve had an abnormal result after a cervical screening test. You may also have a colposcopy if you have symptoms
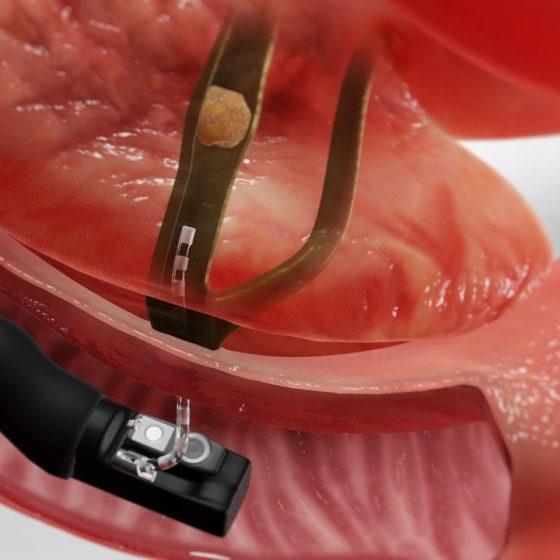
Colonoscopy
A colonoscopy looks at the whole of the inside of the large bowel. A doctor or nurse (endoscopist) uses a flexible tube called a colonoscope. The tube has a small light and camera at one end. The endoscopist puts the tube into your back passage and passes it along the bowel. They can see pictures of the inside of your bowel on a TV monitor. Why might you have a colonoscopy You may need a colonoscopy: to help find the cause of bowel symptoms to look for early signs of bowel cancer as part of the national bowel cancer screening programme
Cholangiography
Cholangiography means looking at the structure of the bile ducts and gallbladder. It can help to find the size of a cancer and whether it has spread. What is cholangiography? Cholangiography means putting a dye called a contrast medium into the bile ducts and gallbladder to show them up clearly on x-ray. Preparing for your test You might have a blood test 2 days beforehand to check how well your blood clots. Tell your doctor if you’re having medicine that changes how your blood clots. This includes: aspirin clopidogrel arthritis medicines warfarin or heparin apixaban, rivaroxaban, dabigatran, edoxaban or betrixaban Your doctor will
Cervical biopsy (cone biopsy)
A cone biopsy is a small operation to remove a cone shaped piece of tissue from your cervix. You usually have it under general anaesthetic, which means you are asleep. The operation takes about 20 to 30 minutes. You will probably stay in hospital overnight. Why you might have a cone biopsy You might have a cone biopsy if you have symptoms that could be caused by cervical cancer. It’s also a treatment for abnormal cervical cells picked up through cervical screening. The abnormal cells might be on the outer surface of the cervix (ectocervix) or the inner part of the cervix (endocervix).
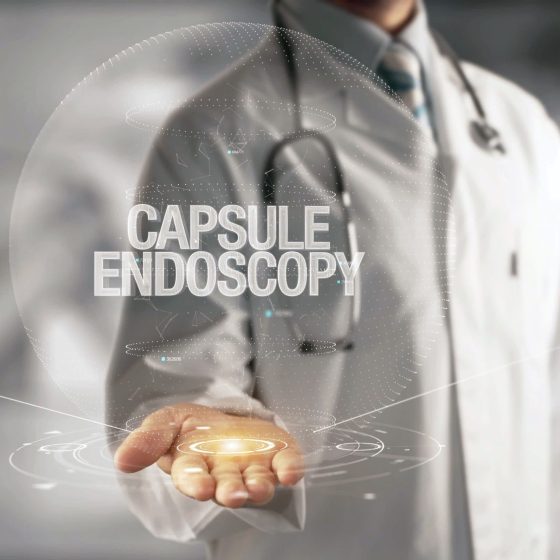
Capsule endoscopy
A capsule endoscopy looks at the inside of your bowel. This is also called a video capsule endoscopy or PillCam. You swallow a capsule that contains a small disposable camera. The capsule is the size of a vitamin pill. The camera takes thousands of pictures as it travels along your gut. The camera sends the pictures wirelessly to a data recorder that you wear on your waist. The test is complete once the capsule has passed through your bowel and out into the toilet. A doctor or specialist nurse looks at the pictures from the data recorder to help find out the
CT urogram
A CT urogram is a test using a CT scan and special dye (contrast medium) to look at the urinary system. The contrast medium helps show up the urinary system more clearly. You have a CT scan of your: kidney bladder tubes that connect the kidneys to your bladder (ureters) A CT scan uses x-rays to take detailed pictures of your body from different angles. A computer then puts them together to make a 3 dimensional (3D) image. CT stands for computed (axial) tomography. It can see details like the soft tissues and blood vessels. You usually have a CT urogram in the x-ray (radiology) department as
CT scan
A CT scan is a test that uses x-rays and a computer to create detailed pictures of the inside of your body. It takes pictures from different angles. The computer puts them together to make a 3 dimensional (3D) image. CT (or CAT) stands for computed (axial) tomography. You usually have a CT scan in the x-ray (radiology) department as an outpatient . A radiographer operates the scanner. The whole appointment can take up to an hour and a half depending on which part of your body they are scanning. You might have a CT scan combined with another test such as
CT colonography
CT (computed tomography) colonography is a test that uses CT scans to check the large bowel (colon) and back passage (rectum). It’s also called a virtual colonoscopy. You have this test as an outpatient in the CT scanning (or radiology) department at the hospital. A radiographer or specialist doctor (radiologist) carries out the test. It usually takes around 30 minutes but you should expect to be in the department for about an hour or so. Why do I need a CT colonography? You usually have this test to help find the cause of your symptoms. Before your test You need
Bronchoscopy
A bronchoscopy is a test to look at the inside of the breathing tubes (airways) in your lungs. You might have this test to allow your doctor to: look for the cause of your symptoms help your doctor see any areas that look abnormal on an x-ray or scans take samples of cells These samples might be a tissue sample called a biopsy. Or your doctor might take some cells by using a small brush or using a liquid to collect them. To have the test your doctor puts a narrow, flexible tube called a bronchoscope down your windpipe (trachea)
Breast ultrasound scan
A breast ultrasound scan is a test that uses high frequency sound waves to create a picture of the inside of the breast. The ultrasound scanner has a probe that gives off sound waves. The probe looks a bit like a microphone. The sound waves bounce off the tissues in your breast, and the probe picks them up. The probe links to a computer that turns the sound waves into a picture on the screen. A specialist healthcare professional called a sonographer usually does the test. When you might have a breast ultrasound scan You might have a breast ultrasound: as a first
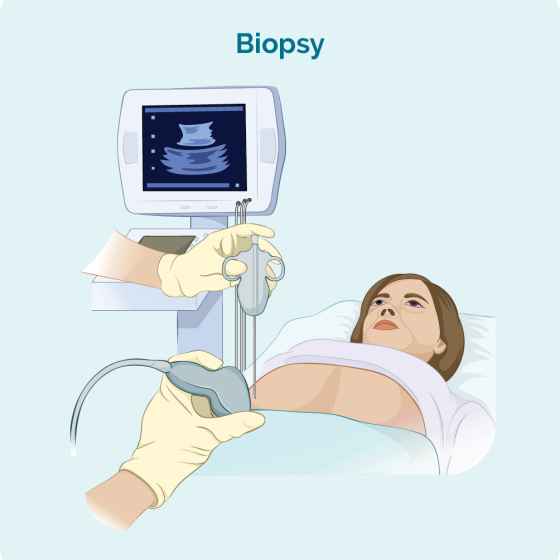
Breast biopsy
A breast biopsy means having a sample of breast tissue taken to look at under a microscope. It is the only way to find out whether you have breast cancer or other breast conditions. Types of breast biopsy There are different types of breast biopsy. The type of biopsy you have depends on a number of factors such as: how big the abnormal area is where it is Before having a biopsy, you have scans such as a mammogram and breast ultrasound scan . Your doctor looks at the results of the scans and decides on the best type of
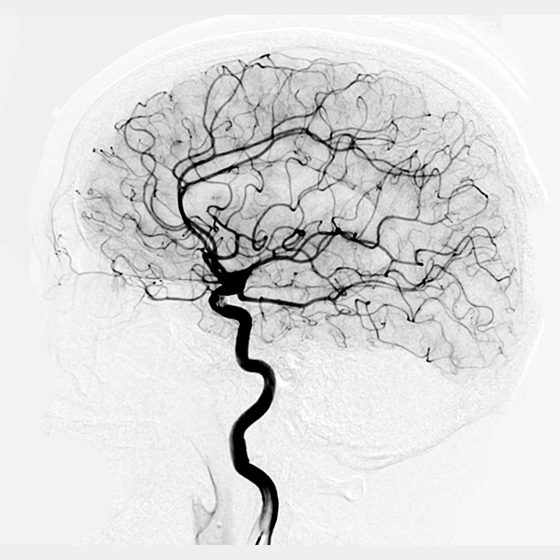
Brain angiogram
An angiogram is an x-ray that can show blood vessels. A specialist doctor called a neuroradiologist injects a dye (contrast medium) and then takes x-ray images of your brain. They look at your brain on the x-ray screen to see: which blood vessels supply the tumour if the tumour is near any major blood vessel This test is also called cerebral angiography. Why you might have it You might have a brain angiogram if: your tumour is growing very deep inside your brain you have a type of brain tumour called meningioma Preparing for your brain angiogram You usually go into hospital on the morning
Bone scan
A bone scan looks for changes in your bones. Before the test you have a radioactive tracer injection into your bloodstream. You have this through a tube (cannula) into a vein in your hand. It takes 2 to 3 hours for the tracer to go around the body. To have the scan you lie down on a couch while the scanner takes pictures. The scan takes 30 minutes to an hour. It is painless and you can go home after the scan. The body gets rid of the tracer through your urine over the next day. A bone scan shows
Bone marrow test
What is a bone marrow test? A bone marrow test is a way of testing cells from your bone marrow. Bone marrow is the spongy tissue inside your bones that makes blood cells. Why do I need it? To find out whether there are any cancer cells in the bone marrow. You might also have one to check whether treatment is working. How do you have it and how long does it take? You have a local anaesthetic injection to numb a small area on your hip. The doctor puts a needle into your hip to suck out some bone
Bone density scan (DEXA, DXA)
DEXA scan stands for dual energy x-ray absorptiometry. It’s also called a bone densitometry scan. It uses low dose x-rays to take measurements to work out the strength (density) of your bones. You have a DEXA scan in the x-ray (radiology) or nuclear medicine department of the hospital. A radiographer does the scan. It takes about 10 – 20 minutes. You’re not enclosed in a small place as the machine has an arm that hangs over the scanning couch. Why might you have a DEXA scan? You might have this scan if you’re having or have had cancer treatment that