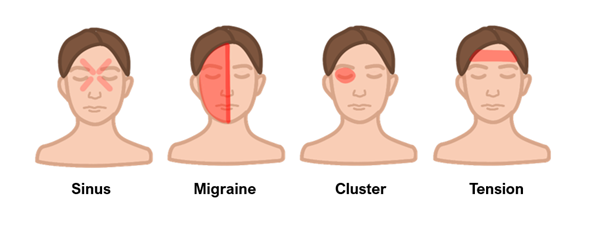
Migraine
This is a primary headache which is more common in women and can be debilitating.
In a migraine, there is an increase in cerebral activity, which releases 5-HT.
This activates the endothelium by binding 5-HT2 receptors causing vasodilation and sensitising nerve endings.
5-HT1D/1B activation inhibits this vasodilation and inflammation of meninges.
A hallmark is that approximately a third are precipitated by an aura, a reversible sensory or motor phenomenon which develops over 5 minutes and lasts < 1 hour. These auras include changes of taste/smell, scintillating scotoma/flashing lights, dysphasia.
Triggers
Alcohol
Menstruation
Bright lights
Stress
Contraceptive pill
Certain foods (cheese, chocolate, red wine, citrus fruit)
Symptoms
Unilateral headache, described as being throbbing in nature
The pain is typically made worse by physical activity
Associated with nausea/vomiting, phonophobia and photophobia
Patients usually go to a dark, quiet room during an attack
Diagnosis
Clinical diagnosis based on the following criteria
i) Must have at least 5 attacks
ii) Headaches last 4-72 hours
iii) Headache has at least 2/4 features: Unilateral, pulsating, moderate or severe pain, worsens with physical activity
iv) Has nausea/vomiting or photo/phonophobia
v) Not due to any other underlying condition
Management
Acute
Medications includes aspirin, paracetamol or ibuprofen.
Take medication at the start of the headache, rather than the aura
5-HT1D/1B agonists such as sumatriptan can also be used
Chronic
If 2 or more debilitating attacks/month, give prophylaxis with propranolol, amitriptyline or topiramate (not used in childbearing women)
If unsuccessful, can consider botulinum toxin injections, calcitonin gene-related peptide (CGRP)-receptor antagonists or occipital nerve blocks.
Tension Headache
This is a recurrent, non-disabling, bilateral headache, which is very common
It can be related to stress and can co-exist with migraine, but of lower severity.
Symptoms
Bilateral low intensity headache described as a “tight band” around head or pressure sensation
Unlike migraine is does not give an aura, change in sensations and is not made worse by physical activity
Key tests
Clinical Diagnosis
Management
For acute attack – Give aspirin, paracetamol or an NSAID
For prophylaxis – up to 10 sessions of acupuncture over 5-8 weeks
Cluster Headache
Headaches which usually occur in groups, over the course of a few weeks in a year.
It is more common in men who smoke and can be precipitated by alcohol.
It is so painful that it is considered to be one of the most severe pain syndromes, inducing acts of self-injury or suicidal ideation.
Symptoms
Sharp, stabbing pain around one eye giving redness, lacrimation
Painful episodes typically last 15min – 190 mins, with quick onset/offset.
There may be 1-2 episodes in a day which come and go in ‘clusters’ lasting 1-3 months
Patient becomes very restless and agitated during episode (pacing around room, not lying down)
Key tests
Clinical Diagnosis
Management
For acute attacks, 100% oxygen or subcutaneous triptan injections
For prophylaxis, give verapamil
Idiopathic Intracranial Hypertension
This is a headache which occurs due to an increase in intracranial pressure (ICP) without a specific underlying cause.
It is usually seen in young, overweight women aged between 20–50 years old.
It is also associated with certain medications (COCP, steroids, tetracyclines).
Risk factors
Overweight
Female
Associated with drugs (pill, steroids and tetracyclines)
Symptoms
Raised intracranial pressure symptoms, (early morning headache, worse lying down, sneezing and bending over)
Bilateral papilloedema with enlarged blind spot
Blurred vision due to pressure on optic nerve
Can lead to vision loss
Ringing in the ears with the heartbeat

Key tests
Lumbar puncture shows raised CSF pressure
Imaging, e.g., MRI is used to exclude a structural cause
Management
Advise weight loss with salt restriction and exercise or bariatric surgery
Diuretics, e.g., acetazolamide is used to reduce ICP
If persistent, consider practical interventions to reduce ICP e.g., lumbar puncture or ventriculoperitoneal shunt.
Medication overuse headache (Rebound headache)
This headache is associated with patients who take chronic analgesic medication.
It occurs for more than 15 days per month and does not have specific features.
It typically develops after 3 months of analgesic use.
The highest risk is with usage of opioids and triptans (taken for ≥ 10 days/month), then paracetamol and aspirin (≥ 15 days/month) followed by NSAIDs (e.g., ibuprofen)
Symptoms
Daily headache associated with a history of medicines, especially opioids or triptans
Key tests
Clinical Diagnosis
Management
Abruptly stop paracetamol/aspirin/NSAIDs, but wean opiates slowly

