Myasthenia Gravis
This is an autoimmune disease caused by autoantibodies against nicotinic acetylcholine receptors (AchR) at the neuromuscular junction (NMJ).
There can be additional antibodies against muscle-specific kinase (MuSK) protein.
It is more common in women and associated with thymus hyperplasia and thymoma.
Symptoms
Use dependent muscle weakness – this worsens with activity and improves with rest
Weakness typically starts with eyes (ptosis, diplopia), and can spread (or generalise) to face, bulbar muscles, neck, trunk, and limbs (proximal > distal muscle weakness)
Symptoms are exacerbated by infections, surgery, and some drugs, e.g., beta-blockers, lithium, certain antibiotics (ciprofloxacin, gentamicin)
Key tests
Blood test shows anti-AChR antibodies, (and anti-MuSK antibodies)
Creatinine kinase is normal, showing the symptoms are not secondary to myositis
EMG shows decreasing response to repetitive nerve stimulation
CT scan imaging can be used to look for a thymoma (tumour of thymus gland)
Management
Anticholinesterases (e.g., pyridostigmine) increase amount of acetylcholine available in the NMJ, therefore improving stimulation of muscles
Immunosuppression e.g., steroids for acute flares
Steroid sparing agents, such as azathioprine, mycophenolate mofetil, rituximab
Thymectomy improves symptoms and may be considered without thymoma in AChRantibody positive disease
Myasthenic crisis
Lambert-Eaton Syndrome
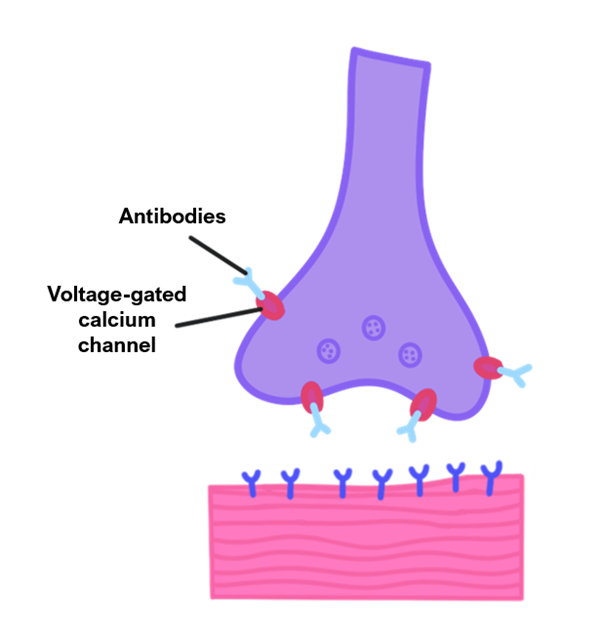
A disease caused by antibodies against presynaptic calcium channels (VGCC).
It can either be autoimmune or secondary to a paraneoplastic syndrome e.g., from small cell lung cancer.
This leads to impaired ACh release, causing less activation of the muscle.
Symptoms
Proximal muscle weakness, with pronounced gait problems.
Strength may improve with use
The lower limbs are affected first and eye/respiratory muscles are usually not affected (or affected late)
Autonomic symptoms – dry mouth, urine retention, constipation
Areflexia (compared to normal reflexes in myasthenia gravis)
Key tests
Blood test shows anti-VGCC antibodies
EMG – motor amplitude increases with muscle contraction
CT scan to check for cancer
Management
If due to cancer, treat the cancer to improve symptoms
Steroids or immunosuppression particularly in autoimmune LEMS
3,4 diaminopyridine (amifampridine) – this blocks K+ channels in nerve terminals to depolarise them opening Ca2+ channels open for ACh release
Motor Neurone disease
This is a disease characterised by the loss of motor neurones from the motor cortex (upper motor neurones) and anterior spinal horn cells (lower motor neurones).
MND very rarely affects eye movement; it does not affect sphincter function and it does not give sensory or cerebellar signs.
There are four clinical patterns of MND, but the most commonly tested at medical school is amyotrophic lateral sclerosis (ALS).
Symptoms
Gives a mixture of upper and lower motor neuron symptoms and signs
LMN signs – flaccid paralysis with muscle atrophy, fasciculations, impaired reflexes
UMN signs – spasticity, rigidity, hyperreflexia, clonus, a positive Babinski sign
Wasting of dorsal hand muscles and tibialis anterior
Also affects bulbar and respiratory function, sometimes at presentation
Key tests
It is a clinical diagnosis based on above symptoms and signs
Nerve conduction studies and EMG
Brain and spinal cord MRI to exclude structural cause
Lumbar puncture is used to exclude an inflammatory cause
Management
Managed by a multidisciplinary team as there is no cure available
Riluzole, an NMDA antagonist is used which improves survival by several months
Non-invasive ventilation improves survival

