Primary Sclerosing Cholangitis (PSC)
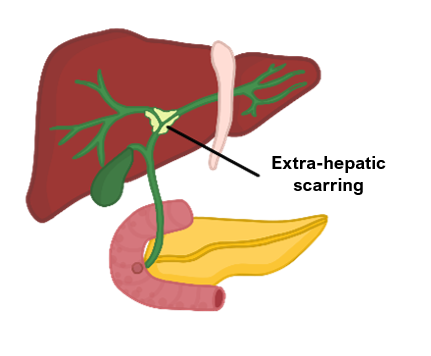
This is a chronic disease characterised by inflammation and scarring of the intrahepatic and extrahepatic bile ducts.
Chronic inflammation leads to “onion-skin” fibrosis narrowing the ducts.
This can result in strictures, causing a backlog of bile which results in jaundice.
Bile is hepatotoxic and progression of the disease leads to liver cirrhosis.
It is classically seen in young men and has a strong association with ulcerative colitis.
Symptoms
Acute obstructive jaundice due to stricture formation
Pruritus, fatigue and RUQ pain
Leads to chronic liver failure
Increased risk of cholangiocarcinoma
Key tests
Liver function tests show raised ALP, bilirubin and mildly raised ALT
Blood tests show raised IgG, ANA and p-ANCA
ERCP/MRCP are diagnostic and show multiple strictures with a beaded appearance
Liver biopsy can be used if there is diagnostic doubt
Management
Ursodeoxycholic acid slows down progression but does not reverse the damage
Liver transplant is the main treatment, but the condition can re-occur after transplant
Primary biliary cholangitis/cirrhosis (PBC)
This is an inflammatory condition which leads to autoimmune destruction of the intrahepatic bile ducts, leading to liver cirrhosis and portal hypertension.
Chronic inflammation leads to granuloma formation, which causes narrowing of the bile ducts resulting in progressive bile stasis. Bile is toxic to hepatocytes and causes degeneration. It then leaks into the systemic circulation resulting in jaundice.
The aetiology is unknown, but it is associated with the presence of antimitochondrial antibodies (AMA) and typically arises in middle aged women.
It is associated with other autoimmune conditions, e.g., Sjogren’s syndrome (most commonly), rheumatoid arthritis and coeliac disease.
Symptoms
Starts with non-specific symptoms, e.g., fatigue, itching
Jaundice in severe cases
Leads to liver cirrhosis with increased risk of hepatocellular carcinoma
Key tests
Blood tests show raised ALP and mildly raised AST/ALT and bilirubin.
Hallmark is raised anti-mitochondrial antibodies (AMA), raised IgM
Liver biopsy can be used if there is diagnostic doubt
Management
Ursodeoxycholic acid slows down progression but does not reverse damage
Cholestyramine to reduce itch
Serial imaging and follow-up blood tests to monitor progression to liver failure
Autoimmune hepatitis (AIH)
This is an inflammatory disease characterised by autoantibodies against hepatocytes.
It is commonly seen in young females arising after an infection or some drugs (e.g., nitrofurantoin) and seen in three main types:
Type 1
This type is seen in adults (usually young women) and children
Associated with raised antismooth muscle antibodies (ASMA) and anti-nuclear antibodies
Type 2
This type only affects children and due to anti-liver/kidney microsomal antibodies (LKM1)
Type 3
This affects middle-aged adults and associated with soluble-liver kidney antigen
Symptoms
Non-specific symptoms (fatigue, jaundice, raised ALT), amenorrhoea in women
Patients can then rapidly show signs of decompensated liver failure, e.g., coagulopathy, jaundice, encephalopathy
Key tests
Blood tests show raised LFTs, presence of autoantibodies and raised IgG
Liver biopsy is diagnostic and shows infiltration of white blood cells in the liver
Management
Immunosuppression (e.g., steroids) or liver transplantation if there is liver failure
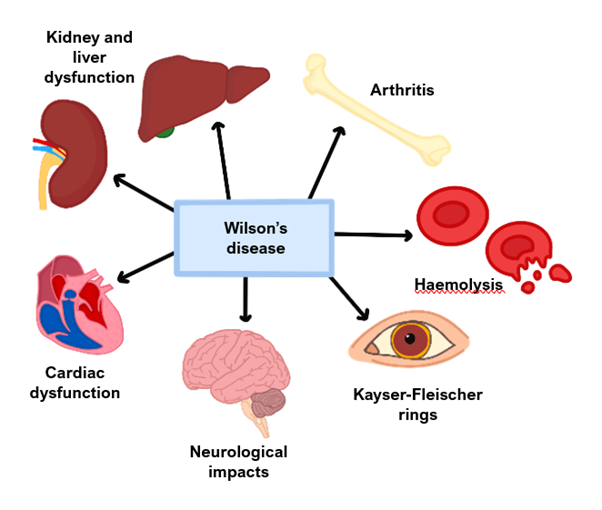
Wilson disease
This is an autosomal recessive condition which occurs due to a mutation in the hepatocyte copper transporter (ATP7B). This mutation increases copper absorption from the small bowel and decreases copper excretion.
As a result, copper is then deposited in places like the liver, eyes, brain and joints.
The condition often develops at an early age (mid-twenties) and leads to both liver and neurological symptoms.
Symptoms
Liver – early onset cirrhosis
CNS – ataxia, asterixis, behavioural changes and psychiatric disturbances
Keyser-Fleisher corneal rings
Blue nails
Key tests
Increased urinary excretion of copper
Low serum copper – it is paradoxically low in this disease
Low serum ceruloplasmin – a serum protein made by the liver which carries copper
Management
1st line is penicillamine (chelator of copper)
Hereditary Haemochromatosis (HH)
This is an autosomal recessive disorder which occurs due to a mutation in the HFE gene, which regulates the transferrin receptor.
It causes increased intestinal iron absorption leading to iron deposition in tissues.
It is more common in European populations and can lead to liver cirrhosis.
Symptoms
Inflammatory symptoms, e.g., fatigue, arthritis
Liver cirrhosis with associated symptoms
Other organ involvement, e.g., diabetes (pancreas), bronzing of the skin, dilated cardiomyopathy (heart)
Key tests
Iron studies – raised ferritin, serum iron and transferrin saturation, low transferrin
If ferritin is raised and transferrin is normal, this suggests that there is Fe2+ overload, which can be secondary to alcohol or liver disease
Genetic testing for HFE gene mutations and liver biopsy are diagnostic
Management
Phlebotomy (regular removal of blood) to keep ferritin levels low and iron chelation
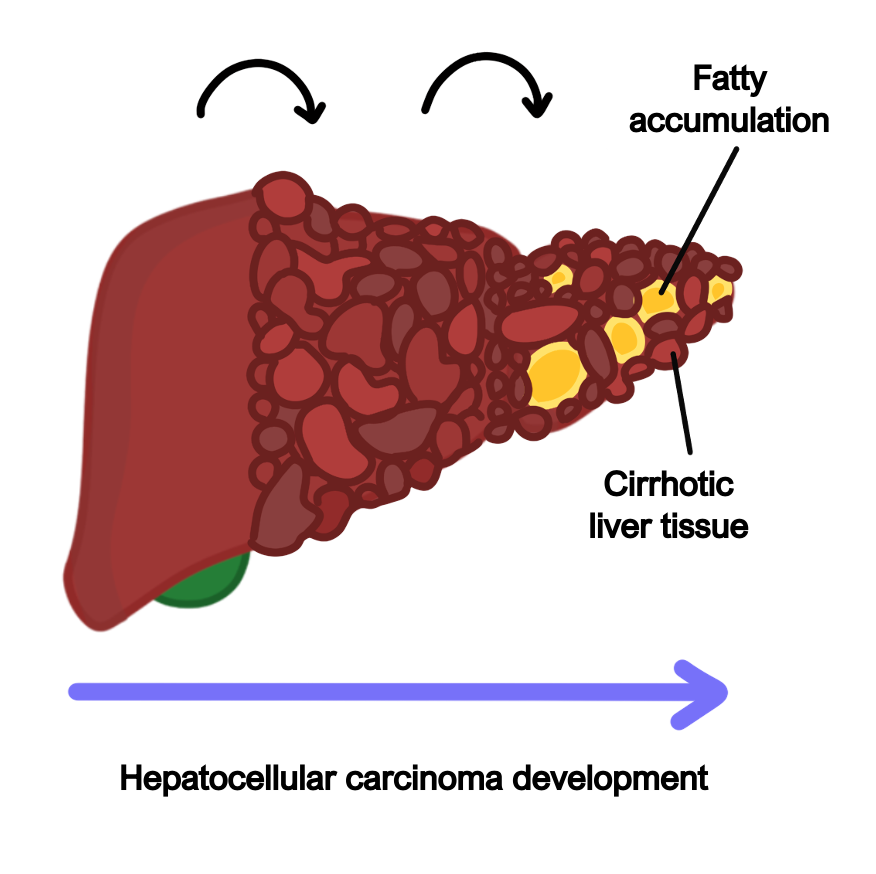
Hepatocellular Carcinoma (HCC)
This refers to a malignant proliferation of hepatocytes and it is the most common type of primary liver cancer. It usually occurs in people with chronic liver inflammation, secondary to conditions including hepatitis B/C and alcoholic liver disease.
It can present as a deterioration from compensated to decompensated liver failure.
Causes
Hepatitis B is the most common cause worldwide
Chronic liver diseases e.g., hepatitis C, alcohol, PBC, PSC, NAFLD
Alpha-1-antitrypsin deficiency, metabolic syndromes
Symptoms
Decompensation of liver failure, e.g., jaundice, ascites, coagulopathy
Weight loss, increased lethargy, loss of appetite, abdominal pain
Presence of a mass in the right upper quadrant
Key tests
Blood tests show deranged LFTs and raised a-fetoprotein tumour marker
CT scan and MRI are imaging of choice
Liver biopsy can be done if there is diagnostic doubt
Management
If suitable, surgical options include resection or liver transplantation
Patients with extensive disease are offered palliative chemotherapy/radiotherapy
People with liver cirrhosis should be screened at regular intervals (every 6 months) with liver ultrasound and alpha-fetoprotein for progression to HCC

