These conditions usually present with epigastric pain. When dealing with stomach conditions you should be aware of the 5 alarm symptoms or age>55years, which require urgent upper GI endoscopy:
Anaemia
Loss of weight
Anorexia
Recent onset symptoms
Malaena/hematemesis
Acute gastritis
This refers acute inflammation of the stomach mucosa, which occurs due to anvimbalance between mucus defence and acid.
The stomach is usually lined by bicarbonate ions, prostaglandins and a mucus barrier,vwhich protects against stomach acid.
The acid damage results in superficial inflammation and can cause erosions (loss ofvsuperficial layer), which may progress to ulcer development (loss of mucosal layer).
Risk factors
Alcohol
Drugs – NSAIDs, steroids
Hiatus hernia
Symptoms
Epigastric pain or discomfort
Vomiting or heartburn
Management
Advice on avoiding alcohol, tobacco, and spicy food
Medical management involves proton-pump inhibitors and histamine antagonists
Chronic Infective Gastritis
The most common form of gastritis, usually due to the bacterium Helicobacter pylori.
This bacterium makes a urease enzyme which breaks down the mucus defence.
This destroys the protective layer and leads to chronic inflammation, which increases the risk for gastric adenocarcinoma and MALT lymphoma.
It can cause epigastric pain and lead to the development of peptic ulcers.
Symptoms
Epigastric pain
Peptic ulcer disease
Key tests
Non-invasive tests are 13C breath test (1st line), stool antigen and serology
Invasive tests are histology (from biopsy) and CLO (campylobacter-like organism) test which can be performed during an OGDpsy)
Management
Triple therapy with 2 antibiotics and proton-pump inhibitors, e.g., PPI (lansoprazole) and amoxicillin and clarithromycin or metronidazole for 7 days
If penicillin allergic, you can give clarithromycin and metronidazole
Chronic autoimmune gastritis
This occurs due to autoimmune destruction of parietal cells which line the stomach.
T cells make antibodies against parietal cells and/or intrinsic factor.
This leads to stomach atrophy. A lack of intrinsic factor can also cause vitamin B12 deficiency, which leads to pernicious anaemia.
Symptoms
Mild jaundice, diarrhoea, sore tongue
Anaemia symptoms, e.g., fatigue, light-headedness, syncope, paleness
Management
Vitamin B12 and folic acid replacement
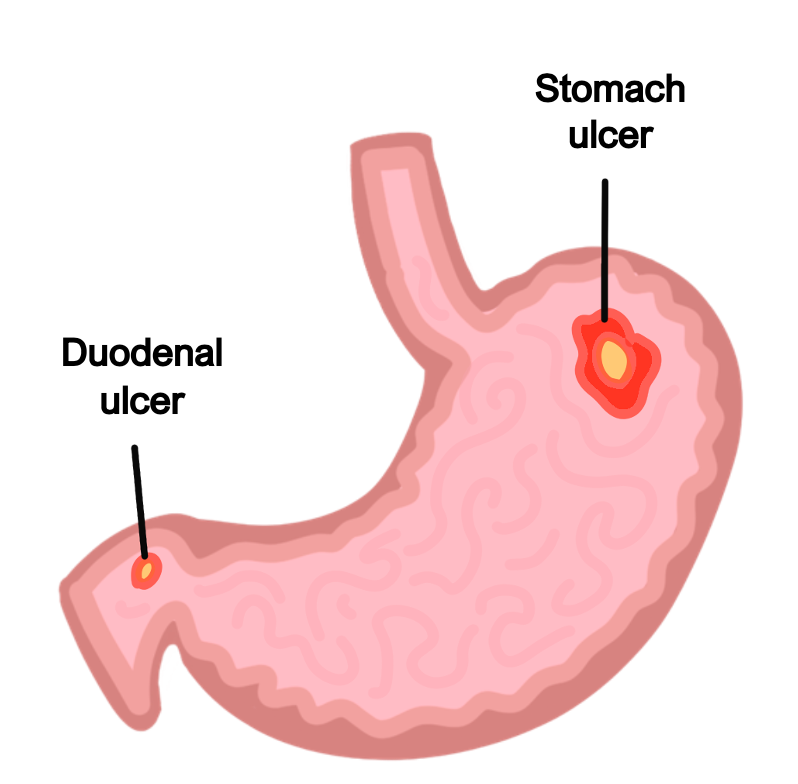
Peptic ulcer disease
This refers to the development of a mucosal ulcer. It is usually found in the proximal duodenum (most common) or the distal part of the stomach.
Duodenal ulcers usually are not malignant, but gastric uclers are associated with gastric cancer.
Duodenal ulcer
This presents with epigastric pain that improves with meals (95% due to H. Pylori)
Usually found in the anterior duodenum.
Posterior ulcers are prone to rupture giving bleeding from gastroduodenal artery, major source of bleeding
Gastric ulcer
This presents with epigastric pain that worsens with meals, risk of bleeding from left gastric
Risk factors
Helicobacter pylori (most common cause)
Drugs – NSAIDs, SSRIs, steroids
Severe burn (Curling’s ulcer) – hypovolemia decreases blood supply to stomach
Raised intracranial pressure (Cushing’s ulcer) – increased vagal nerve stimulation leads to an increase in acid production
Zollinger-Ellison syndrome – a gastrin-secreting adenoma, which leads to increased gastric acid secretion and the formation of multiple peptic ulcers
Key tests
Upper GI endoscopy and biopsy to exclude carcinoma
Check for H. pylori using breath test or stool antigen test
Management
Correct underlying cause, high dose PPI to reduce stomach acid secretion
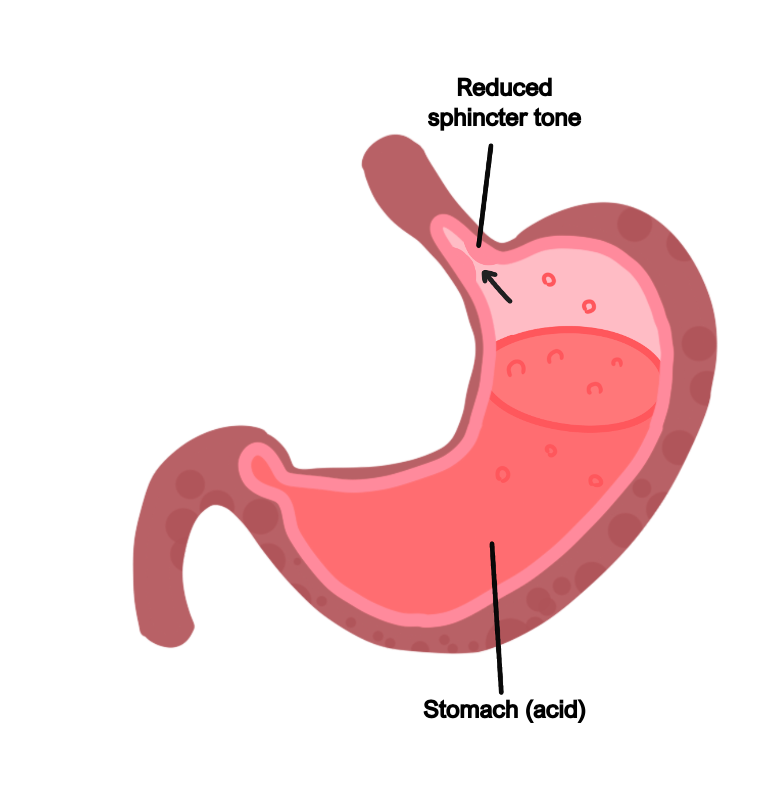
Gastro-Oesophageal Reflux Disease (GORD)
This is a condition which leads to reflux of acid from the stomach into the oesophagus.
It is mostly due to reduced lower oesophageal sphincter tone (idiopathic).
It is also associated with features like obesity and drinking caffeine.
There is also an increased risk in hiatus hernia. This refers to herniation of the stomach above the diaphragm, which usually occurs in overweight patients.
H. pylori eradication is not routinely used in the treatment of GORD.
Causes
Reduced lower Oesophageal sphincter tone (idiopathic)
Obesity
Caffeine
Hiatus hernia – this is herniation of the stomach above the diaphragm, usually in overweight patients
Symptoms
Heartburn, belching (dyspepsia)
Cough, damage to enamel of teeth
Dysphagia is possible but usually no weight loss and patients are systemically well
Can lead to stricture formation and Barrett’s oesophagus (intestinal metaplasia), which increases the risk of developing oesophageal cancer
Complications
Oesophagitis with stricture
Barrett oesophagus – intestinal metaplasia giving risk of Oesophageal cancer
Key tests
Endoscopy if there are red flag (ALARM) symptoms, especially in patients over the age of 55, or for patients in which symptoms persist > 4 weeks despite treatment
If endoscopy is negative, can do 24-hour oesophageal pH monitoring
Management
Encourage weight loss, reduce acid secretion with PPIs
If symptoms persist, surgical options are explored, e.g., laparoscopic fundoplication, a surgery which prevents reflux by wrapping gastric fundus around lower oesophageal sphincter. This is considered after other options have been exhausted.
Gastric carcinoma
This is a malignant proliferation of the surface epithelial cells, which can be divided into two types. These tumours present late and metastasise to lymph nodes, e.g., Virchow’s node (Troisier sign).
Intestinal type
This is more common and presents as a large ulcer usually in antrum
It commonly metastasizes to liver and umbilicus (Giving Sister Mary Joseph Node)
Risk factors
Inflammatory conditions – H. Pylori, autoimmune gastritis
Blood group A
High nitrate diet (Japan)
Diffuse type
This is characterized by signet ring cells that infiltrate gastric wall causing diffuse thickening
Not associated with the previous risk factors
Can metastasize to ovaries (Krukenberg tumour)
MALT lymphoma
This is a gastric lymphoma which is usually due to H. pylori infection.
It can lead to a raised protein level in the blood but has a good prognosis.
It is treated by H. pylori eradication, but if persistent may require chemotherapy.
Symptoms
Weight loss and anorexia
Abdominal pain and dysphagia
Nausea and vomiting
Epigastric mass
Key tests
OGD with biopsy is the definitive investigation
Imaging, e.g., CT or endoscopic ultrasound can be used for staging
Management
Surgical resection of tumour (e.g., gastrectomy), with combination chemotherapy

