Posterior pituitary gland
Diabetes insipidus (DI)
This is a condition characterised by the production of large volumes of dilute urine, which occurs due to poor water reabsorption by the kidney.
Central/Neurogenic DI
This refers to a failure of the pituitary gland to produce ADH.
It can occur idiopathically, due to a congenital defect in the ADH gene or secondary to central nervous system trauma (e.g., following neurosurgery) and tumours.
It is responsive to desmopressin treatment.
Nephrogenic DI
This is when the kidneys are unable to respond to ADH.
This can be due to genetic mutations in the ADH receptor, electrolyte abnormalities, but also secondary to drugs such as lithium and demeclocycline.
It is not responsive to desmopressin.
Dipsogenic DI/primary polydipsia
This is large amounts of urine production secondary to drinking too much water
Symptoms
Polydipsia (e.g., kids drinking bathwater) with life-threatening dehydration
Production of large volume (> 3 L/day) of dilute urine
Key tests
Blood tests – hypernatraemia and high plasma osmolality
Water deprivation test
Water deprivation test
Management
Aim to correct the underlying cause
For central DI, first line is desmopressin
For nephrogenic, bendroflumethiazide can be used as it has anti-diuretic actions
SIADH syndrome
This is a condition which leads to excessive ADH secretion. This leads to high amounts of water reabsorption from the kidney resulting in dilution of the blood.
Causes
Ectopic ADH production (e.g., small cell lung carcinoma)
CNS trauma/tumours
Drugs, e.g., SSRIs, tricyclic antidepressants, PPIs
Symptoms
Low volume, concentrated urine
Hyponatreamia which can lead to cerebral oedema giving headaches and seizures
Key tests
High urinary sodium concentration and osmolality
Blood tests show hyponatraemia (Na < 125 mM), low serum osmolality
Management
Water restriction
Demeclocycline, an antibiotic which reduces sensitivity of the collecting duct to ADH
ADH receptor antagonists e.g., vaptan drug family
Anterior pituitary gland
Hypopituitarism
This refers to decreased secretion of anterior pituitary hormones, which leads to symptoms according to the hormone(s) that are affected.
Causes
Hypothalamus – Kallman’s syndrome, tumour
Pituitary stalk – Trauma, Carotid artery aneurysm
Pituitary gland – Adenoma, apoplexy (bleeding of adenoma, haemorrhage of gland)
Symptoms
Hypopituitarism gives many symptoms due to the effect on the corresponding hormones.
Key tests
Hormonal profile to see which hormones are affected
Management
Hormone replacement therapy
Sheehan syndrome
During pregnancy, the pituitary gland grows larger, but blood supply hardly increases.
High blood loss in childbirth (post-partum haemorrhage) can cause ischaemia and infarction of the pituitary gland, leading to the development of symptoms.
Kallman Syndrome
This is a condition where there is a failure of the development of GnRH neurons derived from olfactory epithelium.
It causes low levels of LH and FSH, resulting in delayed puberty and hypogonadism.
It also causes anosmia (lack of smell), cleft lip and colour blindness.
Pituitary adenoma
This is a benign tumour of the anterior pituitary cells.
It can be a microadenoma (<1cm) or macro (>1cm)
Can also be functional (hormone-producing) or non-functional (silent)
Most common tumour is prolactin secreting –> non-functional –> GH secreting –> ACTH secreting
Symptoms
Double vision, due to pressure on cavernous sinus pressing CN III, IV and VI
Bitemporal hemianopia, due to compression of the optic chiasm
Raised intracranial pressure if large, leading to nausea/vomiting, headaches
If hormone-producing, it presents with additional symptoms based on the type of hormone produced
Key tests
Pituitary blood profile (GH, prolactin, ACTH, FH, LH and TFTs)
MRI provides visualisation of the pituitary tumour
Management
Medical management of the hormones affected
Definitive treatment is removal of tumour. Options include surgery (e.g., transphenoidal hypophysectomy) and/or radiotherapy for residual/recurrent adenomas
Hyperprolactinemia
This refers to raised prolactin levels in the blood.
In addition to direct effects on lactation, raised prolactin inhibits GnRH which decreases testosterone and oestrogen giving secondary effects like osteoporosis.
Causes
Most often due to a pituitary adenoma increasing prolactin production
Reduced inhibition of pituitary gland, e.g., secondary to dopamine antagonists
Conditions which increase oestrogen e.g., pregnancy, polycystic ovary syndrome
Associated with acromegaly (1/3 of patients)
Primary hypothyroidism, as TRH stimulates prolactin release
Symptoms
As well as direct effects on lactation, raised prolactin inhibits GnRH which decreases testosterone and oestrogen giving secondary effects like osteoporosis.
| Females | Males |
| Amenorrhea – absence of menstruation | Erectile dysfunction |
| Infertility – due to Inhibition of GnRH | Loss of libido |
| Galactorrhoea | Galactorrhoea |
Key tests
Blood tests show raised prolactin levels
Imaging, e.g., MRI is used if pituitary adenoma suspected of pituitary gland
Management
Dopamine agonists to reduce secretion, e.g., bromocriptine/cabergoline
If unresponsive to medical management, surgery can be offered
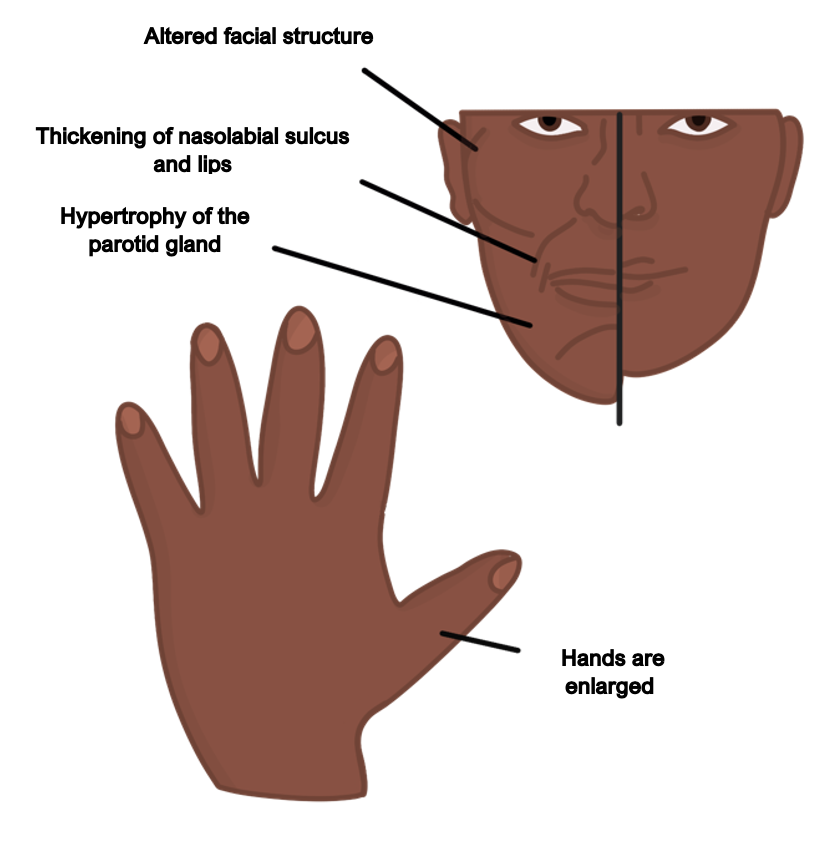
Acromegaly
This is a condition characterised by an increased secretion of growth hormone from the pituitary gland. It is most commonly due to a pituitary adenoma.
GH stimulates bone and soft tissue growth through IGF-1.
Symptoms
Can cause gigantism due to increased bone growth (if occurs in childhood)
Enlargement of the hands, tongue, jaw, and feet (increase in shoe size)
Acroparathesia (tingling in the hands and feet)
Pituitary tumour features, e.g., headache, visual disturbances, hyperprolactinaemia
Excessive sweating and oily skin, due to sweat gland hypertrophy
Complications
Growth of visceral organs can lead to cardiomyopathy
Hypertension
Secondary diabetes mellitus as growth hormone induces gluconeogenesis
Increased risk of colorectal cancer
Key tests
Blood tests – raised serum IGF-1 levels
Oral glucose tolerance test can be used:
Normally, GH levels are suppressed by the administration of glucose. In acromegaly there will be reduced suppression of growth hormone levels.
MRI pituitary fossa is used for imaging of the tumour
Management
Definitive management is surgery to remove the pituitary tumour
Octreotide is a somatostatin analogue, used as adjunct to surgery
Radiotherapy can be used in older patients or those not suitable for surgery
If above options are unsuccessful, pegvisomant (GH receptor antagonist) can be used

