Type 1 Diabetes
This is a condition in which there is autoimmune destruction of pancreatic beta-cells leading to an inability to produce endogenous insulin.
T lymphocytes attack the islets and autoantibodies against insulin can be present.
It is associated with HLA-DR3 and HLA-DR4.
The disease usually manifests in adolescence, sometimes after a viral infection.
Symptoms
Polyuria, polydipsia, and glycosuria, due to hyperglycaemia
Weight loss, as unopposed glucagon leads to lipolysis and glycogenolysis
Can be asymptomatic and lead to life threatening complications
Management
The mainstay of treatment is insulin to control blood glucose levels
Insulin regimes vary according to patient’s diet, their ability to comply with medication, age and whether they can self-administer insulin
A common regime is basal-bolus: this involves long-acting insulin (e.g., insulin glargine) once a day and short-acting insulin (NovoRapid) before each meal
Metformin, can be added if BMI > 25 kg/m2
Glucagon kit, given to patients in case of hypoglycaemic crisis
Daily glucose monitoring. Patient are advised to check before and approximately 2 hours after each meal as well as
Longer term management involves checking the HbA1c every 3–6 months and monitoring for complications including retinal screening, diabetic foot screen and renal function.
Type 2 Diabetes
This is the most common form of diabetes, which occurs due to end-organ insulin resistance which is the most common form of diabetes.
It usually arises in middle-aged, obese adults. This is because poor glucose control and hyperglycaemia over a long period causes downregulation of insulin receptors.
Eventually, the beta-cells become exhausted which results in insulin deficiency.
It is associated with obesity, lack of exercise, alcohol excess.
There is a higher incidence in Asians and male sex.
Causes
Obesity, lack of excessive
Alcohol excess
Stronger genetic influence than type 1 – high in Asians, men and the elderly
Symptoms
Initially clinically silent, but then similar complications to type 1 in later disease
Key tests
The diagnosis of diabetes mellitus is made using plasma glucose or a HbA1c sample.
If asymptomatic, you need 2 readings on 2 separate occasions to diagnose T2DM:
Fasting glucose > 7.0 mmol/L or random glucose/OGTT > 11.1 mmol/L
HbA1c > 48 mmol/mol (6.5%)
Management
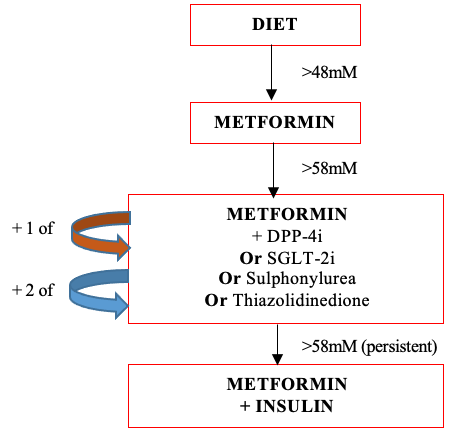
1) If HbA1c rises to 48 mM
Trial lifestyle modifications such as diet, weight control and exercise
2) If HbA1c stays above 48 mM
Start metformin and aim for HbA1c < 48 mM. Also give SGLT-2 inhibitor if QRISK > 10%, heart failure or cardiovascular disease
3) If HbA1c rises > 58 mM
Add sulphonylurea or DPP-4 inhibitor or thiazolidinedione or SGLT-2 inhibitor
4) If HbA1c stays > 58 mM
Add 3rd drug (metformin + 2 of previous options)
5) If not effective/tolerated and BMI > 35 kg/m2
Switch one of the 3 drugs for a GLP1 mimic
6) If still not controlled, commence insulin therapy (but continue metformin)
Other Diabetes Types
Latent autoimmune diabetes of adults (LADA)
This is a form of type 1 DM, but with slower progression to insulin dependence in later life.
Maturity Onset Diabetes of the Young
This is usually due to an autosomal dominant mutation in the HNF1A gene.
It leads to poor insulin production, causing T2DM symptoms in younger patients.
Management involves giving sulphonylureas to increase insulin release.
Gestational diabetes
This is a transitory form caused by pregnancy associated hormonal changes
Prediabetes
This is a term used for patients who do not meet the diagnostic criteria for diabetes but are likely to develop the condition soon.
It is defined as a HbA1c of 42–47 mmol/mol or fasting glucose of 6.1–6.9 mM.
These patients should be offered lifestyle and dietary advice to reduce the risk of developing diabetes.
Secondary diabetes
This refers to diabetes (HbA1c > 48 mM) that is a consequence of other conditions that affect blood glucose and/or insulin sensitivity:
Pancreatitis, causing damage to insulin producing cells
Acromegaly, due to excess of growth hormone
Cushing’s disease, due to cortisol excess or secondary to steroid use
Hyperthyroidism, associated with increased insulin resistance

