Thyroid Gland
The thyroid gland is an endocrine gland in the neck. It is made of two lobes joined together by an isthmus.
It is made up of two types of cells which control metabolic rate and calcium levels in the body.
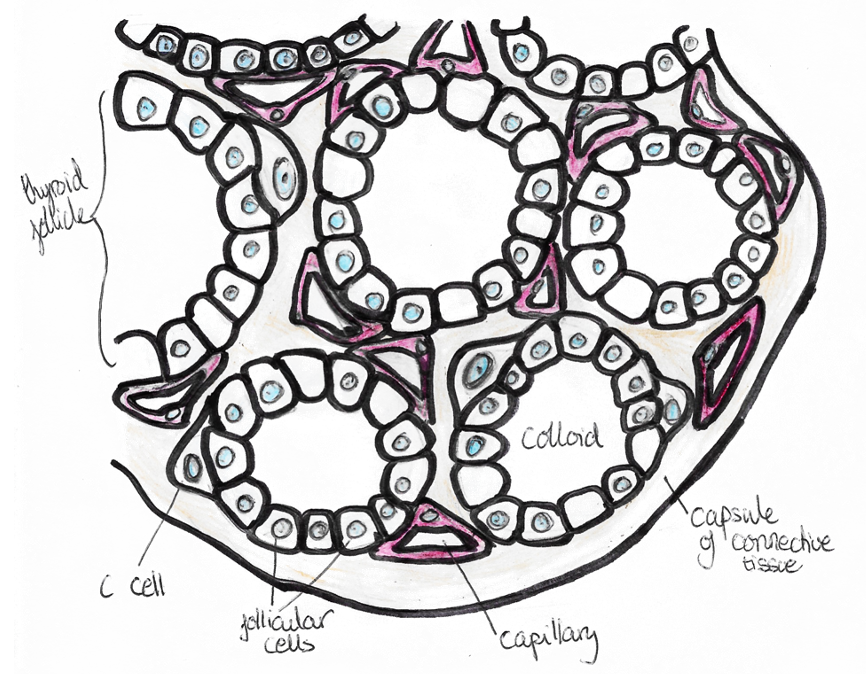
a) Parafollicular cells
– Secrete Calcitonin, which antagonizes effects of PTH
– Decreases plasma [Ca2+] by decreasing bone breakdown by inhibiting osteoclasts whilst promoting osteoblasts
b) Follicular cells
– Produce thyroid hormones, triiodothyronine (T3) and thyroxine (T4) – tyrosine based hormones partially composed of iodine.
– Mainly produces T4 which is 5x less active than T3 – 85% of T3 is made from peripheral conversion of T4
Thyroid hormone synthesis:
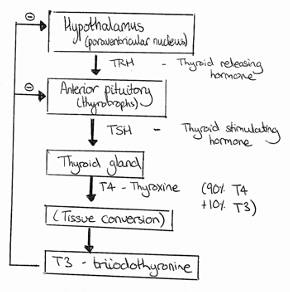
Hypothalamus releases thyrotropin releasing hormone (TRH) which stimulates Thyroid stimulating hormone (TSH) and prolactin from anterior pituitary.
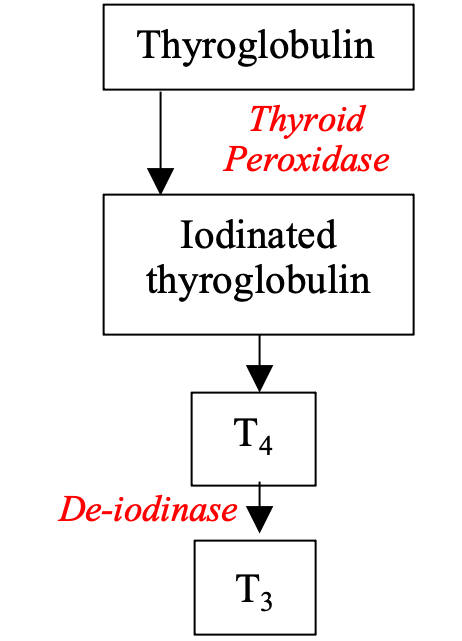
– Thyroid hormone is made in follicles by the iodination of tyrosine residues from a precursor called thyroglobulin, using the enzyme thyroid peroxidase.
– This is iodinated with 2 iodides to give T4 which can then be deiodinated to T3 by the enzyme 5’-deiodinase
– Control of synthesis is from the hypothalamus via the HPT axis.
– T3 exerts short and long negative feedback loops self-regulating release.
Thyroid hormone actions
Thyroid hormones travel in the blood bound to thyroxine binding globulin.
– T4 converted to T3 by enzyme deiodinase –> T4 has a half-life of 7 days, but T3 is only 1 day
– These bind thyroid hormone receptors in the nucleus of all cells, which initiates transcription of specific genes to exert many different effects:
i) Metabolic – Increase basal metabolic rate of all tissues
– Increase body sensitivity to catecholamines (e.g. adrenaline)
– Increase absorption in the gut and uptake of cells
– Increase glucose and fat breakdown and free fatty acids
ii) Cardiovascular – Increase rate/strength of heartbeat + breathing
– Increase heat generation and body temperature
iii) Development – Facilitates growth rate with growth hormone
– Facilitate normal brain development in fetus and early life
iv) Sexual function – Maintain sexual function, sleep and thought
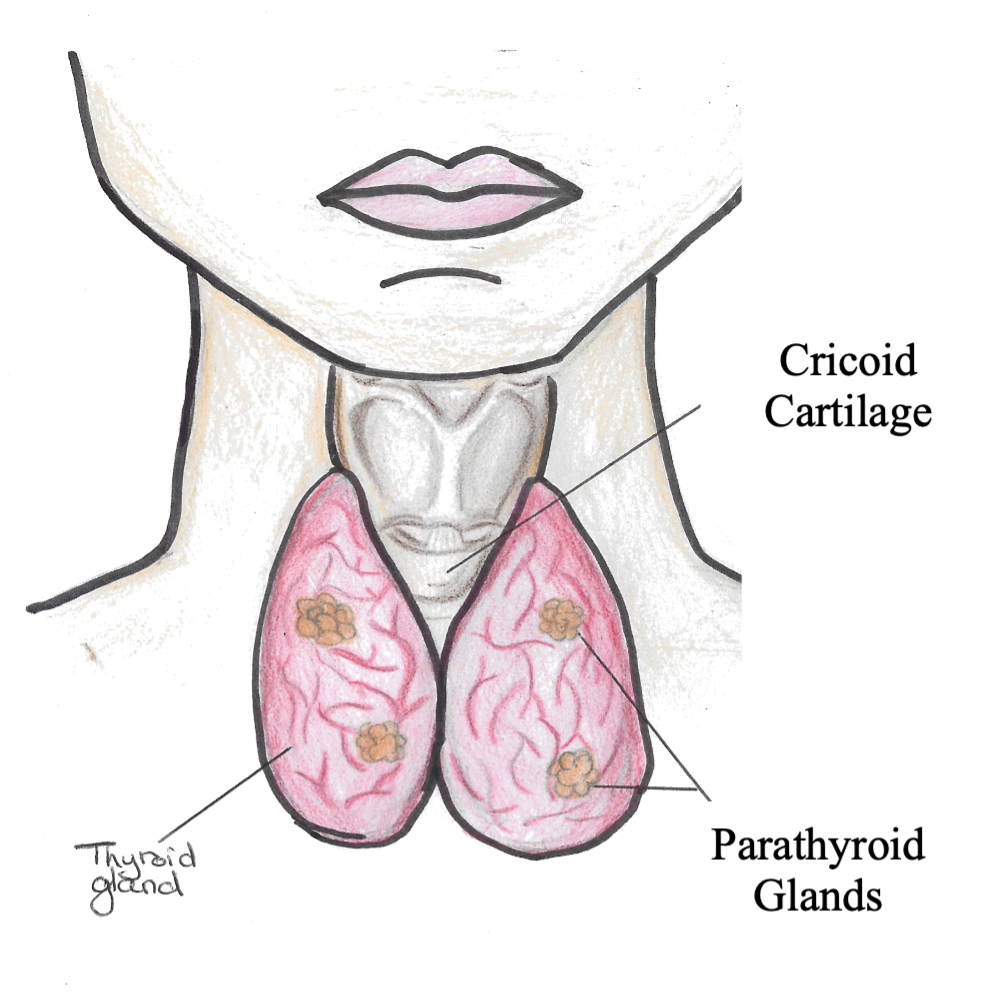
Parathyroid gland
The Parathyroid Glands are 4 tiny glands that are located behind the thyroid in the anterior mediastinum.
Function: Maintain the body’s calcium and phosphate levels
– This is achieved through the secretion of Parathyroid Hormone (PTH)
Release: Secreted in response to decreased plasma Calcium
Actions: PTH acts on the bone and the kidney.
– Increases [Calcium] by stimulating bone resorption by osteoclasts and reabsorption by kidney.
– Causes a net decrease in Phosphate by increasing phosphate excretion by kidney despite bone resorption.
Regulation of calcium homeostasis
The kidney also regulates calcium, which is important as it makes bones and affects resting membrane potential.
– This is because Calcium stabalises sodium channels on the cell membrane decreasing their excitability
– A decrease in calcium reduces threshold for action potentials – increases excitability of neurones.
– Free [Ca2+] extracellular = 1mM, intracellular = 0.1mM
Calcium cocentration is regulated by 3 hormones:
1) Parathyroid hormone:
– PTH is secreted by the parathyroid glands in the neck
– Acts to raise plasma [Ca2+] and lower [Phosphate]
– Has actions both on bone and the kidneys
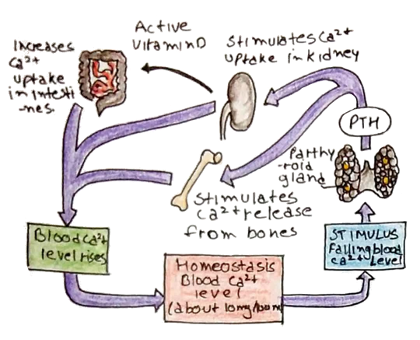
Action on bone
– PTH inhibits osteoblast activity and instead stimulates osteoclasts
– Results in the breakdown of bone releasing free [Ca2+] into the blood.
Action on kidneys:
– In the DCT, PTH increases PKA, which increases levels of NCX
– This increases the transport maxima for [Ca2+] absorption, increasing [Ca2+] in the blood
– PTH decreases transport maximum for reabsorption of phosphate. The decreasing phosphate conc. favours dissolution of calcium causing a rise in ECF free [Ca2+].
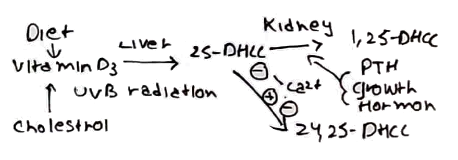
2) 1,25-DHCC:
– Derived from vitamin D3 which is broken down in 2 reactions to 1,25-DHCC
– Acts synergistically with PTH to promote bone dissolution
– Increases reabsorption of calcium and phosphate from the kidney and the small intestine to raise the plasma concentration of both.
3) Calcitonin:
This is secreted by the parafollicular cells of thyroid cells
– Inhibits osteoclast activity favouring osteoblast activity
– Acts to decrease ECF free [Ca2+], antagonizing PTH and 1,25-DHCC
– It is important during pregnancy to protect maternal bone and lactation
Hypercalcaemia:
– Usually due to hyperparathyroidism and malignancy (bony metastasis)
– Raised Ca2+ decreases excitability of cells
– Classically leads to groans (lethargy, pain)
+ stones (calcium deposits) + psychiatric moans
– First line treatment is to administer fluids
Hypocalcaemia:
– Most commonly due to hypoparathyroidism
– This increases excitability of cells giving signs:
e.g. Trousseau sign – inflating cuff above systolic BP –> reflex muscle contraction
Chvostek sign – tap on zygomatic bone –> twitching of facial muscle as it is more excitable

