Eczema (Dermatitis)
This is the general term which describes a condition which causes general inflammation of the skin.
Atopic Eczema (Atopic dermatitis)
This is the most common type of eczema and most common inflammatory disease of early childhood
– It affects about 20% of children under 5 and 2% of adults
– It is an immunologically mediated inflammatory skin reaction, mediated by increased Th2 cells
– This promotes pathogen specific IgE antibodies (type I hypersensitivity) increasing eosinophils and mast cells
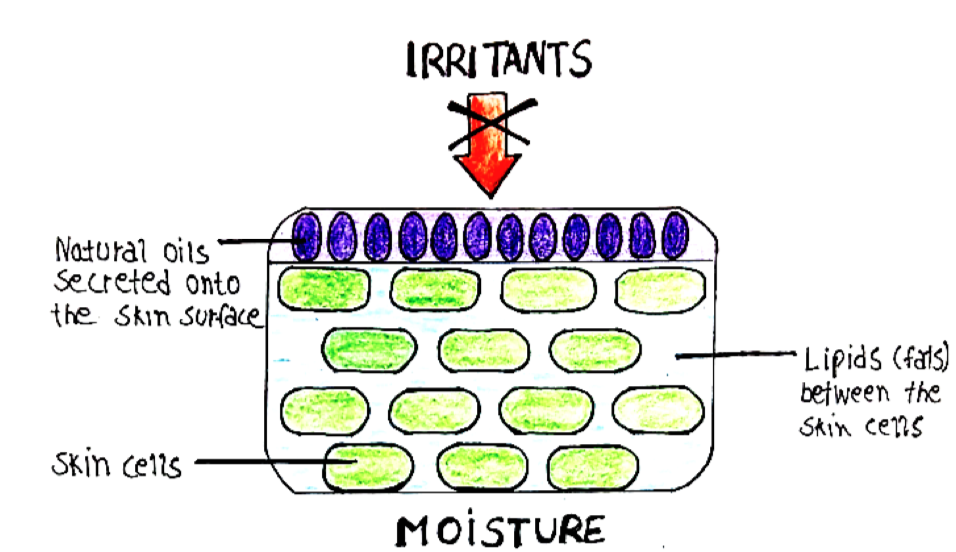
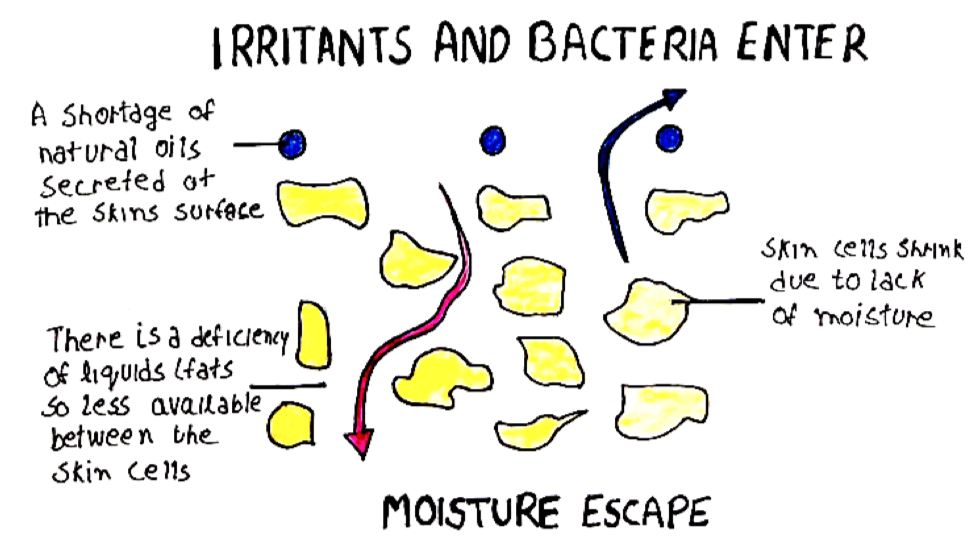
Cause: Underpinned by a genetic defect in skin barrier function
– Associated with a loss of function variant of protein filaggrin.
– This leads to decreased ceramide lipids in skin leading to breakdown of skin barrier and escape of moisture
– This allows irritants to enter and activate inflammasomes.
Risk Factors:
a) Atopy – associated with a family history of atopic conditions
– Often get eczema first, then asthma and rhinitis
b) Diet – exacerbated in infants due to allergy to egg/cow’s milk protein
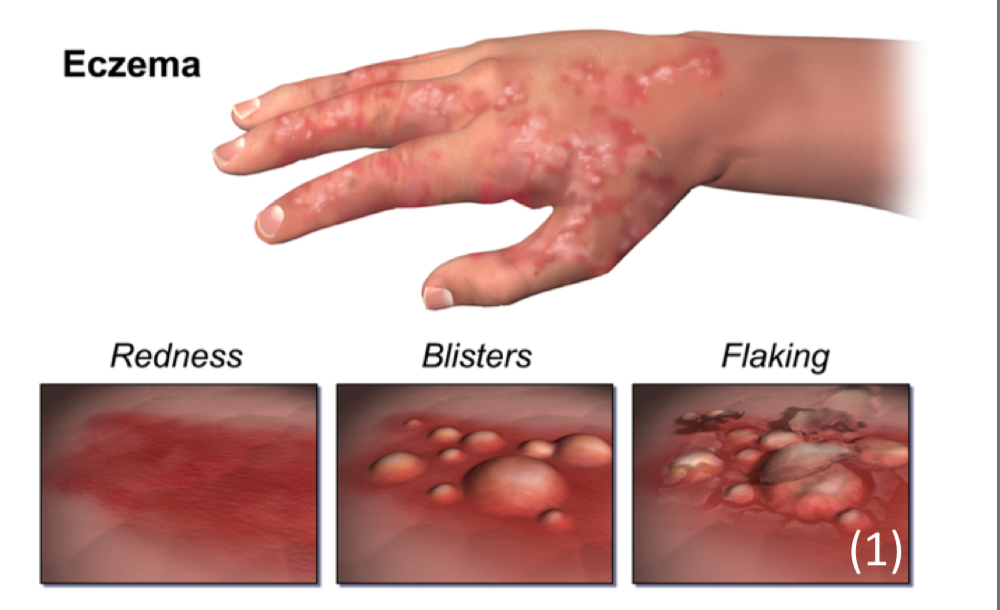
Appearance:
– Erythematous, indistinct fissuring (cracks) through the epidermis
– For babies, lesions more concentrated around the face and the torso. – As children get older, lesions are more likely to be found in the flexor surfaces (elbows, behind knees) and the creases of the face.
– This is because sweat concentrates here causing more irritation.
Management:
i) Emollients
– These are liquids which are water based, aim to restore barrier function and flush our irritants
– Examples include Hydromol and Diprobase
– Prescribed in a ratio of 10:1 with a topical corticosteroid
ii) Topical steroids – 1 fingertip unit (FTU) = 0.5g treats area twice that of human adult hand:
- Hydrocortisone (Mild strength)
- Eumovate (moderate) – a corticosteroid called clobetasone
- Betnovate valerate (Potent)- contains the active compound betamethasone
- Dermovate (very potent)
- Fucidin H – This is a mixture of hydrocortisone + fusidic acid, used if the lesions are also infected
iii) Topical Calcineurin inhibitors – Tacrolimus may be used in severe eczema, as it has immunosuppressive action.
iv) Phototherapy – Used in severe eczema
Discoid Eczema.
A type of eczema with round or oval erythematous patches.
– It is seen in any age but more common in adults, seen in the arms and legs
– The rash starts off as a group of red spots which eventually merge together in a red round patch and become very itchy
Management – Mild topical steroids

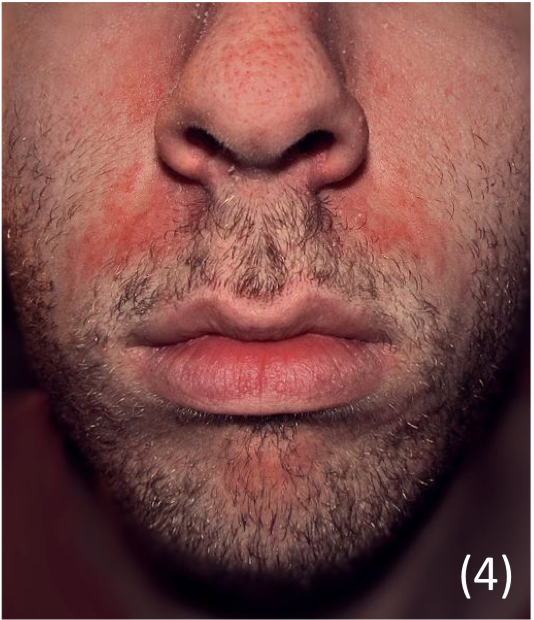
Seborrheic eczema/dermatitis
This is a common, chronic type of dermatitis that primarily affects parts of the body which are rich in sebum, such as the scalp and face.
– It is thought to be due to an abnormal response to the fungus Malassezia furfur, which can lead to inflammation in the skin.
– It can affect both infants and adults giving rise to various symptoms.

i) Infants –> Usually seen in small children younger than 3 months
– It classically gives lesions with a yellowish-scale on the scalp (cradle-cap)
– Also affects axilla and groin areas giving a pink patchy rash which is not very itchy, so the baby is likely not to be perturbed by the rash.
Management
– Regular washing with shampoo to clear scales
– If more severe, topical antifungal cream (ketoconazole)
ii) Adults –> This usually starts in the late teens but is also seen in the elderly.
– Affects sebum rich areas (scalp, nasolabial areas, periorbital, behind ears)
– Gives pink thin scaly plaques in the folds which improve in summer (not itchy)
Management
– For acute flare, mild topical steroids
– For scalp, medicated shampoo
– For body, topical antifungal cream (ketoconazole)
Eczema herpeticum
This is a skin infection which is caused by the herpes simplex virus 1+2.
– Children/infants will classically have a history of atopic dermatitis, which then can rapidly progress into eczema herpeticum.

Appearance
– Leads to extensive crusted papules, and blisters, which can bleed
– Can be filled with clear yellow fluid or pus-like matter
– Swollen lymph glands and fever
– If untreated can start to affect the eyes, brain and lungs
Diagnosis
– Clinical diagnosis (if doubt take swab and do PCR sequencing of viral DNA)
Management
– A dermatological emergency –> Admit to hospital + Acyclovir
– If there is eye involvement, refer to ophthalmology
Contact dermatitis
This refers to inflammation of the skin which occurs due to direct contact with an agent, leading to redness, dryness and fissuring.
– It is the most common occupational skin disorder, and seen in populations of cleaners, food workers and hairdressers (wearing gloves).

Appearance
– Often seen on the hands due to direct contact (glove distribution)
– Erythema and itchiness, with drying/flaking of the skin
– Gives thickened skin with swelling, but crusting/vesicles are rare
Management
– Improve hand routine –> Avoid soap, wear better gloves
– Can prescribe topical steroids and ensure frequent emollient use.
Dyshidrotic Eczema (Pompholyx)
This condition is characterised by blisters on the fingers, palms and soles of feet
– No known cause but related to seasonal allergies and stress and seen in adults
Symptoms
– Starts as intense itching and burning of the skin on hands and fingers
– Forms large painful blisters which flake off
– Lasts up to 3 weeks before they dry off and heal
Management
– Moisturise + Topical Corticosteroids

