In addition to cardiac output, the arterial blood pressure is dependent on the resistance within the circulation.
– This is mainly affected by the diameter of the arterioles, which contain smooth muscle in their walls.
– The arterioles are capable of constricting and dilating but can be abnormally affected by the presence of atherosclerosis and also which narrow/occlude vessels.
Normal control
The arterioles contain a lot of smooth muscle in the tunica media of their walls.
– The contractile system of smooth muscle is more complicated as smooth muscle cells do not contain troponin.
– An action potential generated allows Ca2+ ions to enter –> binds calmodulin –> binds caldesmon allowing actin myosin cross-bridges to form
–> Increased phosphorylation of myosin light chain by MLCK –> increases cross bridge cycling
In exercise
During exercise, we have to ensure that blood is diverted away from non-essential organs like the gut, skin and kidneys, whilst increasing supply to skeletal muscle and the heart.
Increase Na in periphery –> binds a2 receptors on peripheral arterioles
–> These are Gi coupled –> less phosphorylation of myosin light chain kinase –> increased cross-bridges –> vasoconstriction
– Increase in Na inheart/skeletal muscle –> bind B2 receptors
–> These are Gs coupled ➔ PKA ➔ phosphorylation of MLCK ➔ vasodilation
Whilst we strive to maintain low peripheral resistance, this can be increased through the presence of atherosclerosis (fatty deposition into the tunica intima of arteries) and clot formation.
Normal clot formation:
Haemostasis is a physiological response to tissue injury in order to prevent blood loss. It is accomplished by the cooperation between platelets, clotting factors and endothelial cells.
– After injury to the endothelium, ECM is exposed and binds platelets via Won Willebrand factor
– Activated platelets promote vasoconstriction and form a primary haemostatic plug using cell adhesion molecules, such as the aIIb/b3 integrin.
The injury to the endothelium can also activate the coagulation cascade – a series of proteolytic reactions in which zymogens are sequentially activated.
Thrombin catalyses the conversion of fibrinogen into fibrin monomers, which polymerize to make a clot.
– These work with platelets to form a stable secondary haemostatic plug.
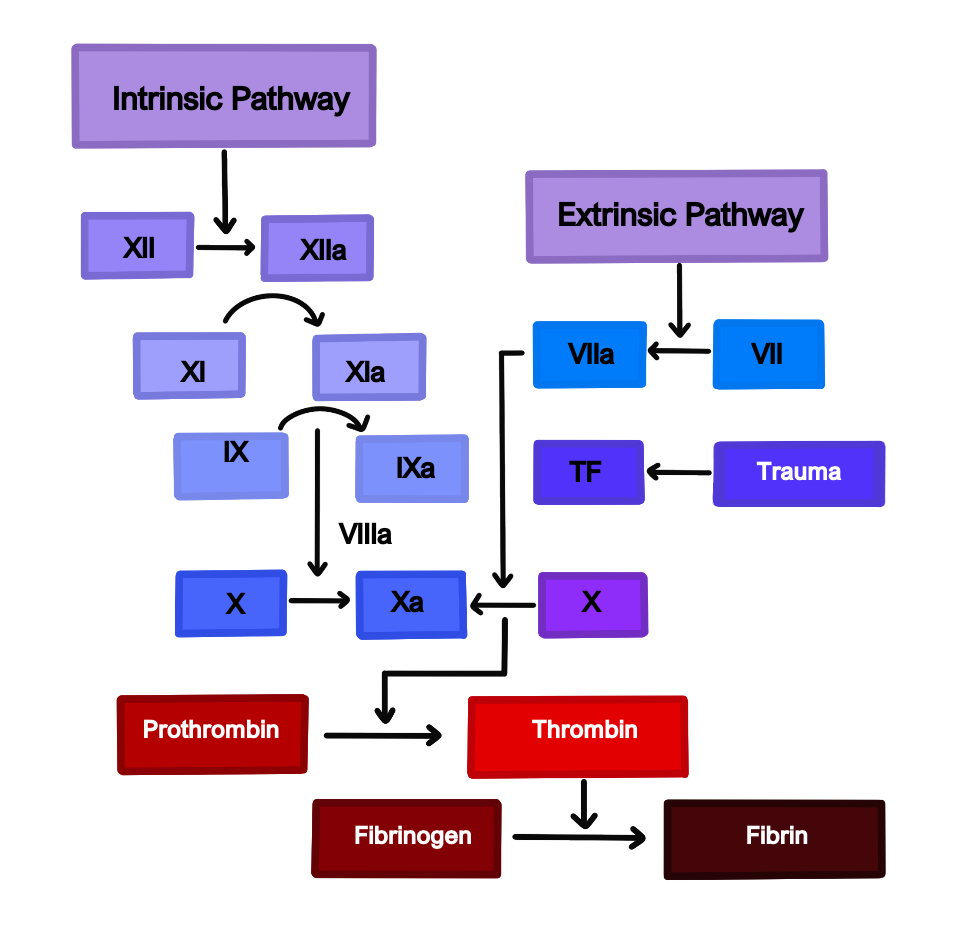
Most coagulation is mediated via the extrinsic pathway, due to tissue factor binding to factor VII.
– The intrinsic pathway plays a minor role.
Clotting function is measured using the INR scale.
– Gives ratio of time taken for person’s blood to clot: compared to normal clotting time.
– If a patient is on warfarin, INR is around 2-3
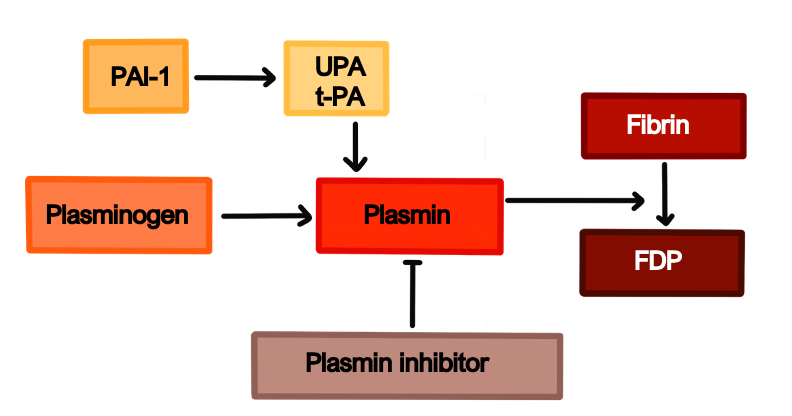
The plamin pathway is activated simultaneously with the fibrinolytic system which works in the opposite fashion:
– Most anti-clotting medicine work by producing the serine protease plasmin
– Plasmin cuts the fibrin mesh at various places producing fragments that can be cleared by kidney/liver
– Also breaks down other clotting factors.
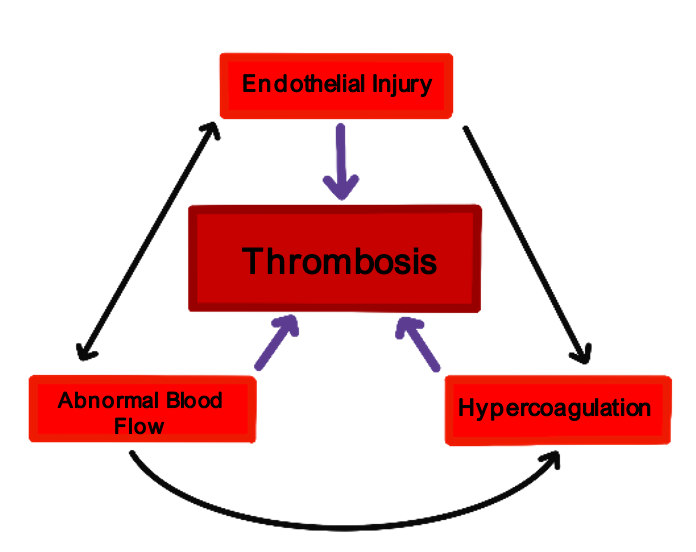
Virchow’s Triad
The chances of a thrombus occurring depend on three types of factors, known as Virchow’s triad:
1) Changes in blood constituents:
These lead to an increased tendency to coagulate
–> Can be genetic – deficiency of antithrombin III or protein C resistance (Factor V Leiden)
–> Acquired – malignancy, smoking, hyperlipidaemia, oral contraceptive pill
2) Changes in vessel wall:
This is due to endothelial cell injury or activation
–> Ischaemia hypoxia
–> Infection
–> Immunological damage (due to immune complexes)
3) Changes in blood flow:
Turbulent flow puts platelets in contact with endothelium and leads to poor delivery of anticoagulants and activation of endothelium
– In arteries –> narrowing, heart valve disease, aneurysm, dysrhythmias
– In veins –> right sided heart failure, varicose veins, increased viscosity
Atherosclerosis
This refers to a deposition of fatty substances in the tunica intima of arteries and arterioles. Arterial walls consist of 3 main layers:
– Tunica intima – endothelial cells linked by tight junctions
– Tunica media – contains layers of elastic tissue and smooth muscle cells
– Tunica adventitia –connective tissue, nerves, lymphatics and vasa vasorum vessels supplying artery.
It takes a series of steps to develop atherosclerosis:
1) Endothelial cell activation
2) Monocyte infiltration into plaque:
–> Monocytes enter and mature into macrophages. They take LDLs and are converted into foam cells
3) Smooth muscle activation:
–> The smooth muscle cells proliferate and migrate into the intima from the media
4) Lipoprotein infiltration:
–> LDL becomes in plaques by Reactive Oxygen Species
5) T cell migration into the plaque
Atherosclerosis Risk Factors
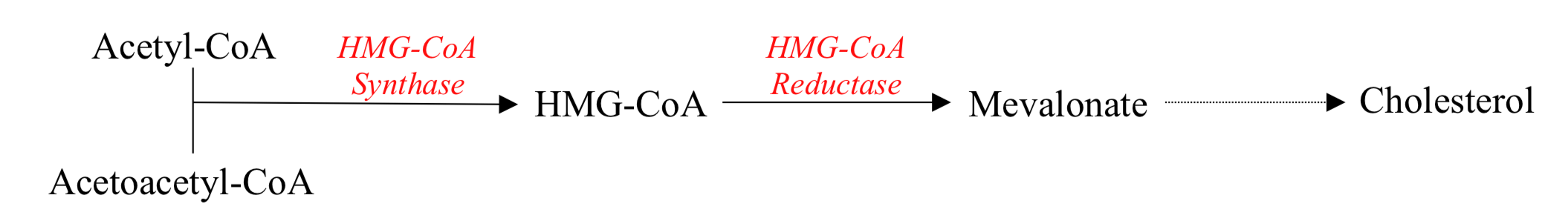
Cholesterol Synthesis
Transport Pathway
Cholesterol is transported around the blood in lipoproteins, which are composed of a cholesterol core, covered by phospholipids cover and apolipoproteins.
– Liver utilizes cholesterol to synthesis bile salts – can be synthesized or uptaken from the blood.
– Hepatocytes have LDL receptors on the plasma membrane to uptake LDL by receptor mediated endocytosis.
– Bile = cholesterol + bile salts, secreted into duodenum
– Bile is reuptaken into the enterohepatic circulation – this is topped up with newly synthesized cholesterol or uptaken from blood LDL

