Overivew
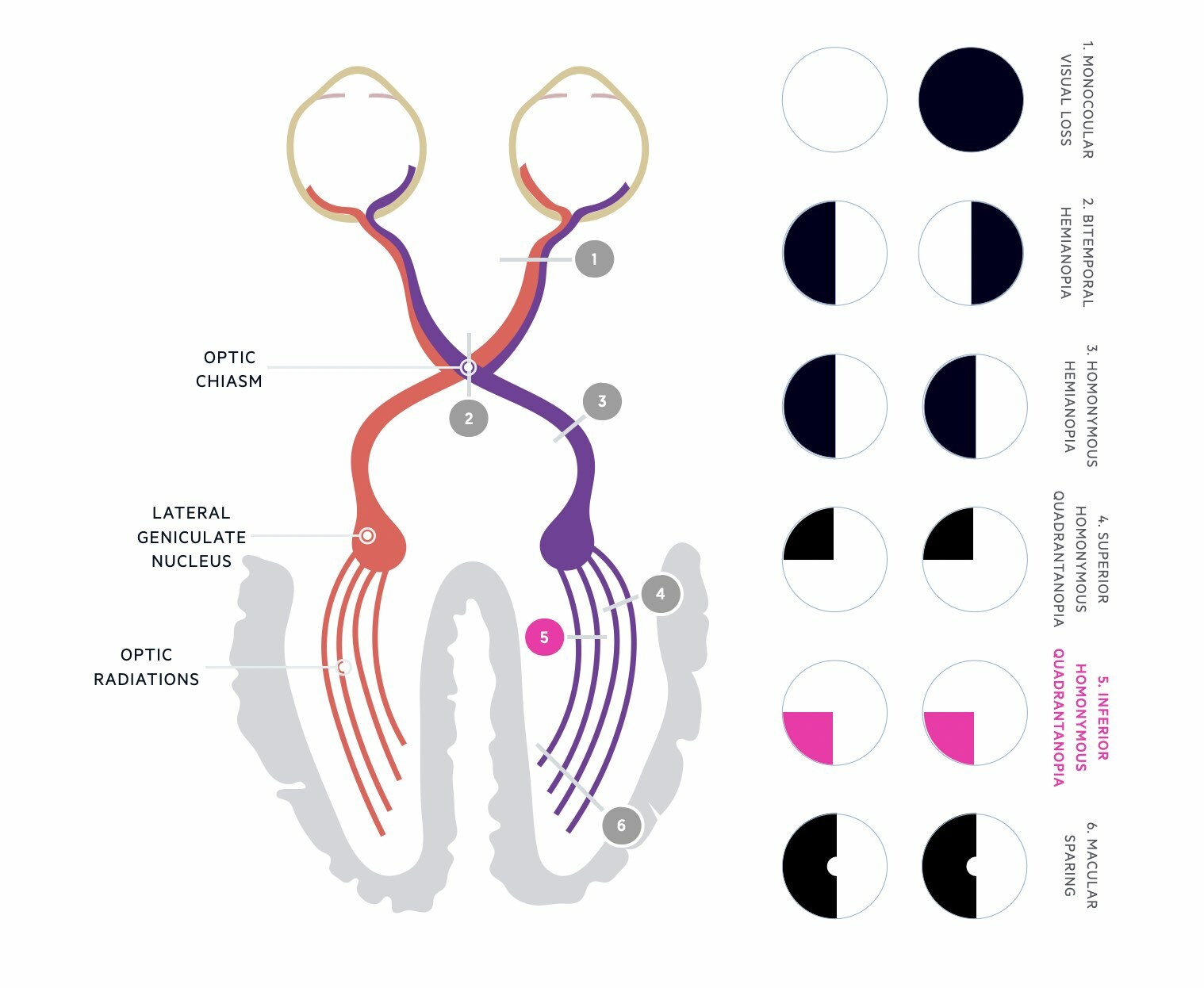
A visual field defect is a loss of part of the usual field of vision.
The visual field describes the area that can be seen by an individual with their eyes fixed on a single point. Our normal field of vision is typically 135º vertically and 180º horizontally (160º for monocular vision). The visual fields can be divided into two components:
- Left visual field: detected by the right temporal retinal fibres (outer) and left nasal retinal fibres (inner)
- Right visual field: detected by the left temporal retinal fibres (outer) and right nasal retinal fibres (inner)
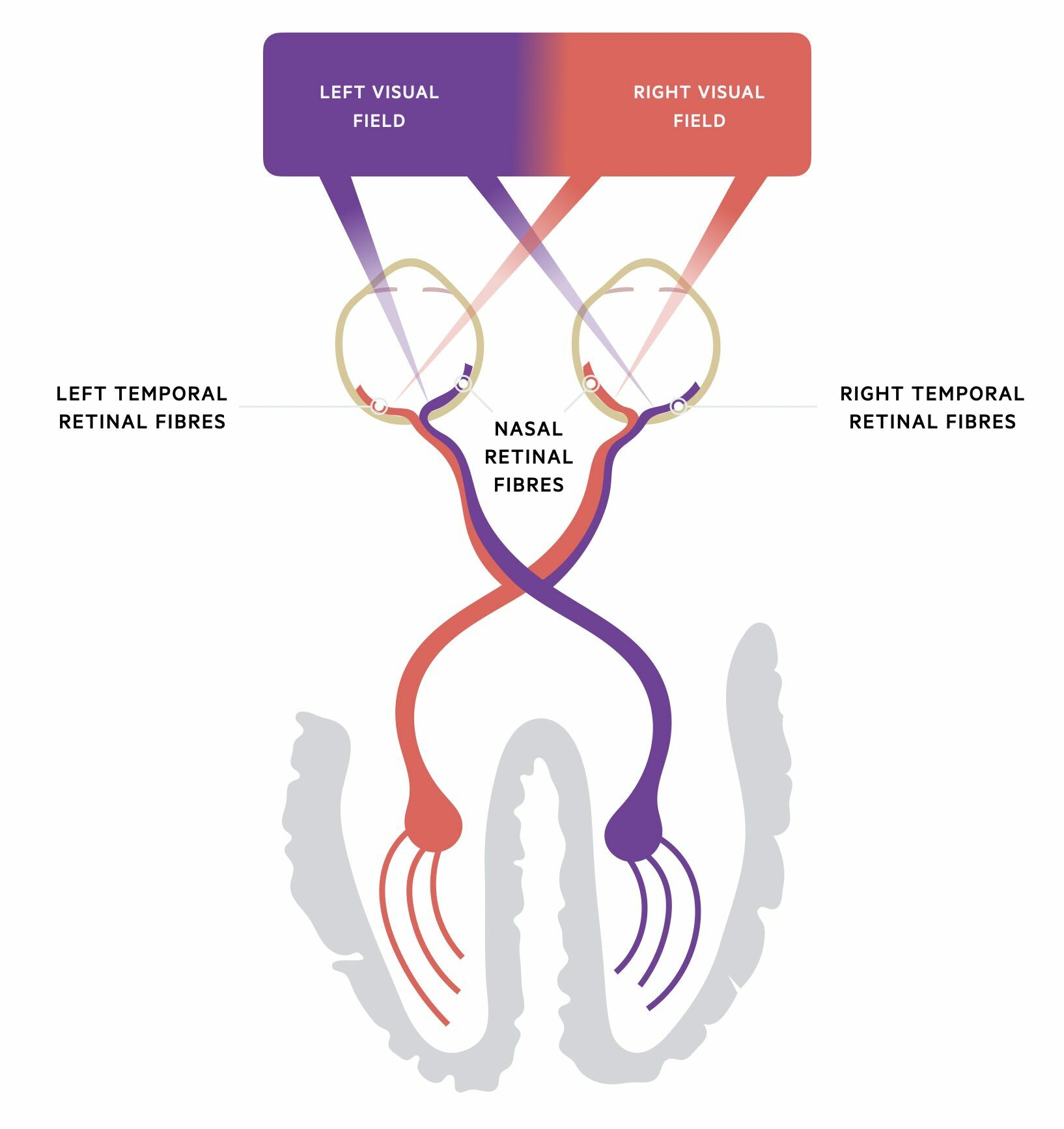
The nasal fields of vision from each eye overlap in forward gaze. Therefore, when assessing visual fields, it is important to assess each eye individually. Information from the visual field is obtained from specialised retinal ganglion cells in the retina, which transmit information via the optic nerve to the occipital lobe for processing.
When there is loss of part of the usual field of vision it is known as a visual field defect. Damage anywhere along the visual pathway from the retina to the occipital lobe can result in visual field defects.
Optic nerve
The optic nerve is the second cranial nerve (II) that transmits visual information from the retina to the visual cortex.
The optic nerves are paired structures that carry sensory information from ganglion cells located within the retina of each eye. It is considered the second cranial nerve but is actually part of the central nervous system. Its fibres are myelinated by oligodendrocytes and encased within the meninges (three membranes that encase the brain and spinal cord).
The optic nerve is made up of >1 million myelinated axons of the retinal ganglion cells that can sensory information from the retina to the primary visual cortex in the occipital lobe.
The optic nerve is divided into four components:
- Optic nerve head: most anterior component located in the eyeball. Corresponds to the blind spot in the visual field
- Intraorbital part: passes from the posterior eyeball to the start of the optic canal
- Intracanalicular part: passes through the optic canal within the lesser wing of the sphenoid
- Intracranial part: joins with the contralateral optic nerve to form the optic chiasm
The ophthalmic artery, which is a branch of the internal carotid artery, is the major blood supply to the optic nerve.
Optic chiasm
The optic chiasm is an important location where retinal fibres of the optic nerve cross over (i.e. decussate).
The optic chiasm has an ‘X’ shaped appearance and is located inferior to the hypothalamus and superior to the sella turcica that is the boney structure that contains the pituitary gland. Therefore, it can become compressed by pituitary tumours.
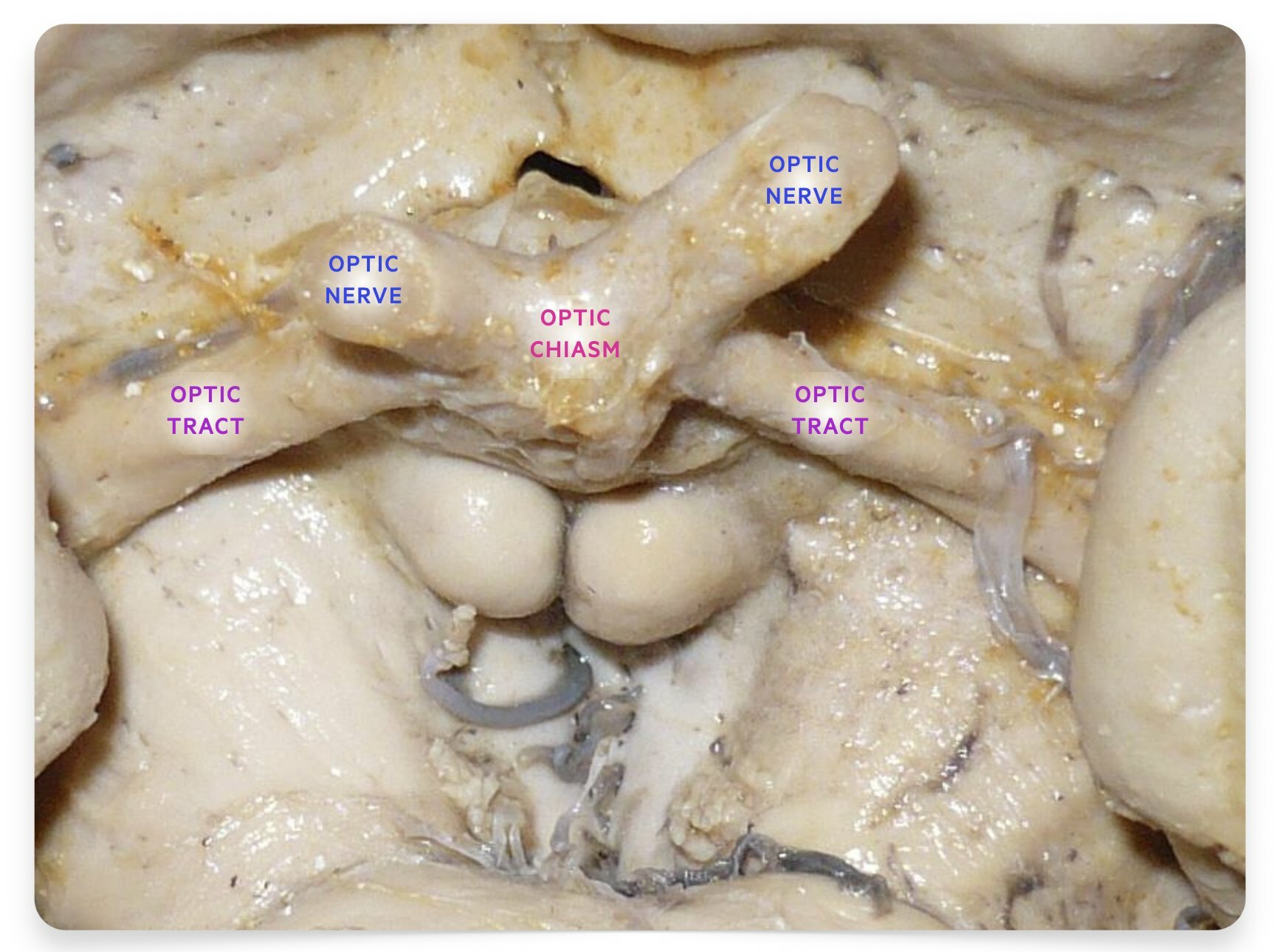
Dissection specimen showing optic chiasm, optic nerves and optic tracts
Image courtesy of Anatomist90, Wikimedia Commons
The optic chiasm is an important location due to the crossing over (i.e. decussation) of optic nerve fibres.
- Nasal retinal fibres: cross at the optic chiasm to join the temporal fibres on the other side
- Temporal retinal fibres: do not cross at the optic chiasm and joined by the nasal fibres from the other side
Beyond the chiasm, the nasal and temporal fibres continue as two distinct optic tracts (right and left). Crossing ensures information from both eyes concerning the same part of the visual field passes to the same area of the visual cortex. The right optic tract corresponds to the left visual field and the left optic tract corresponds to the right visual field.
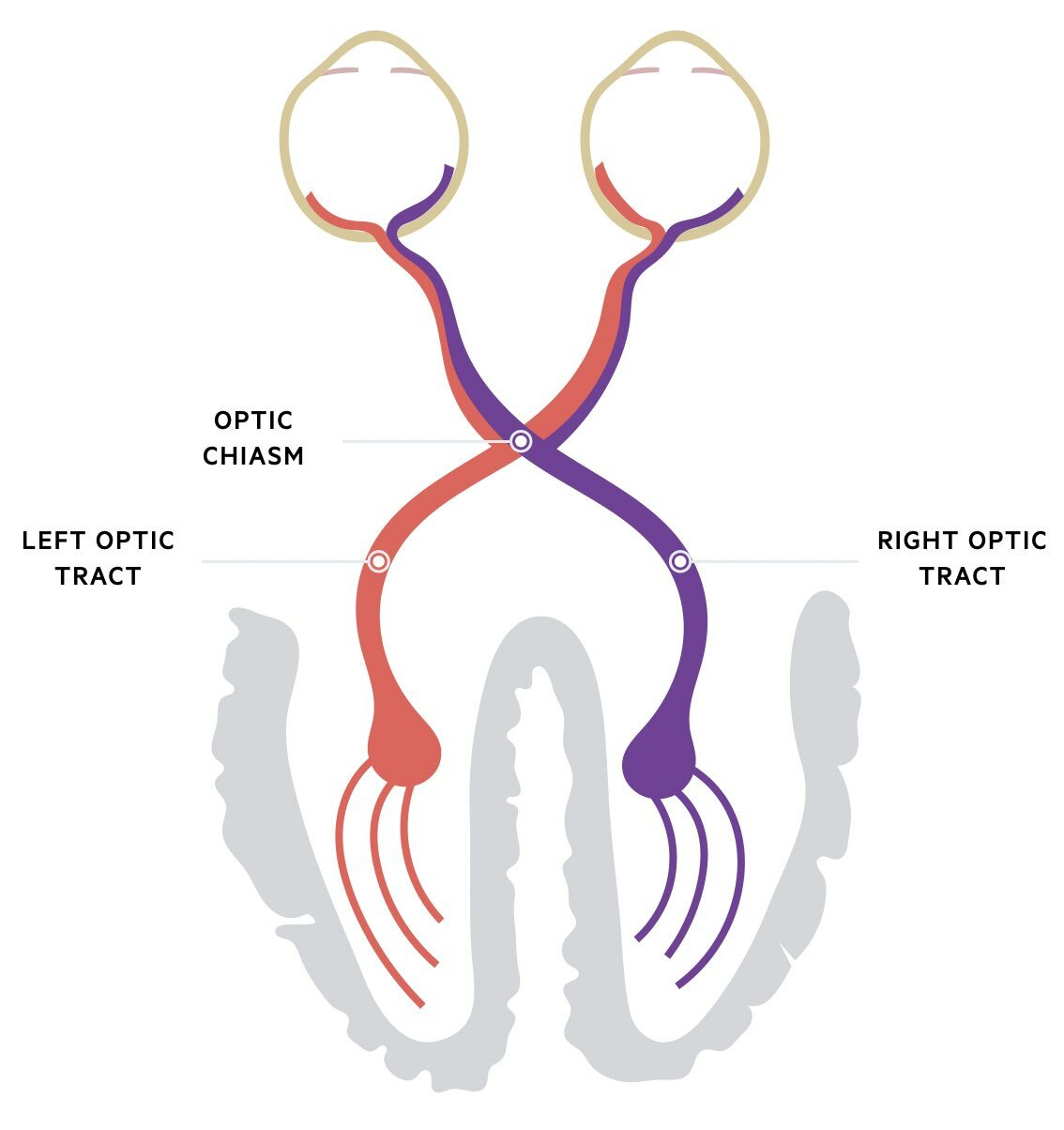
Optic chiasm and optic tracts
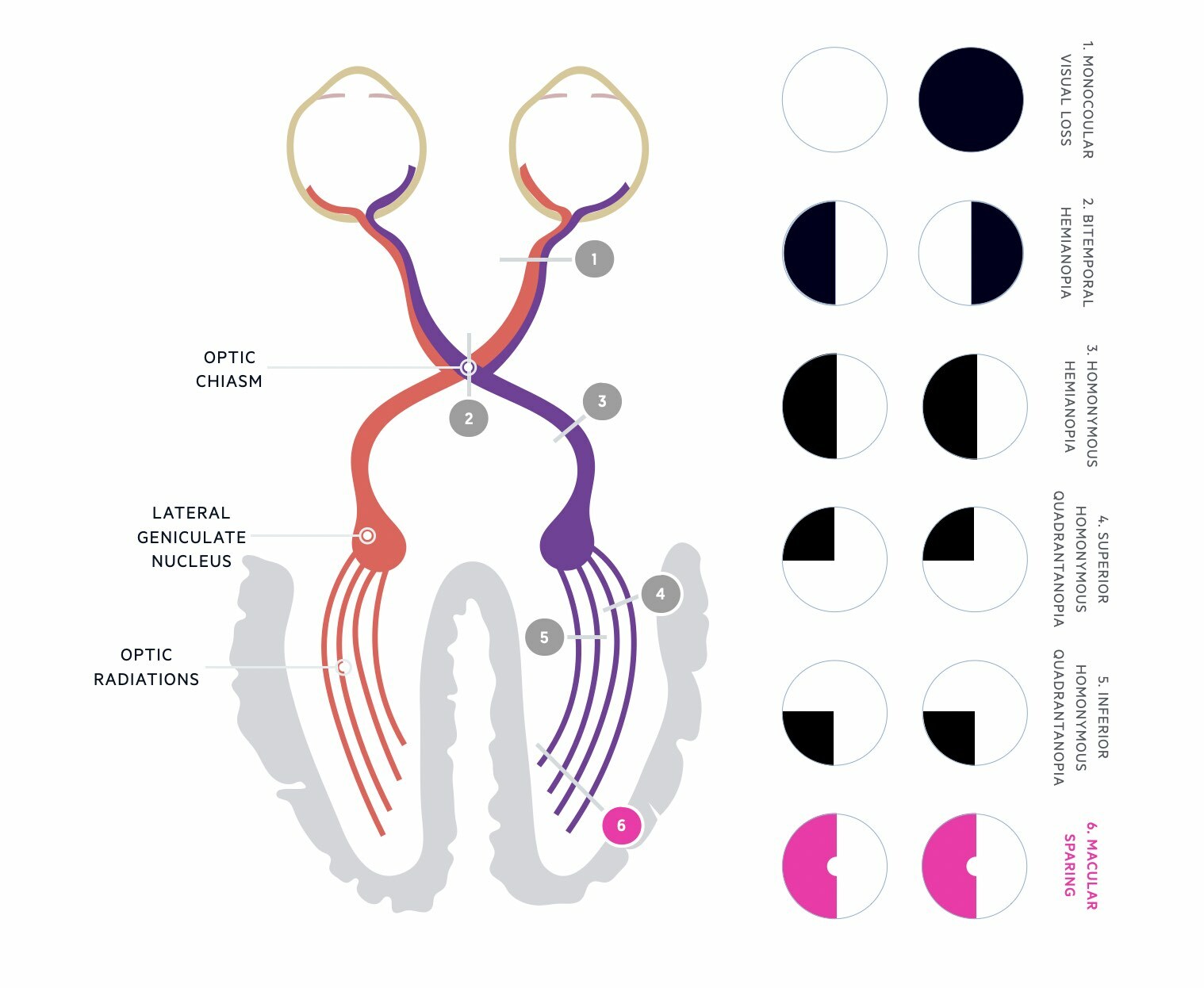
Visual pathway
The visual pathway refers to the structures that are responsible for perceiving, relaying, and subsequently processing visual information.
The visual pathway describes the path of visual information from the retina to the visual cortex in the occipital lobe. It is divided into several components:
- Retina
- Optic nerve
- Optic chiasm
- Optic tract
- Optic radiations
- Visual cortex
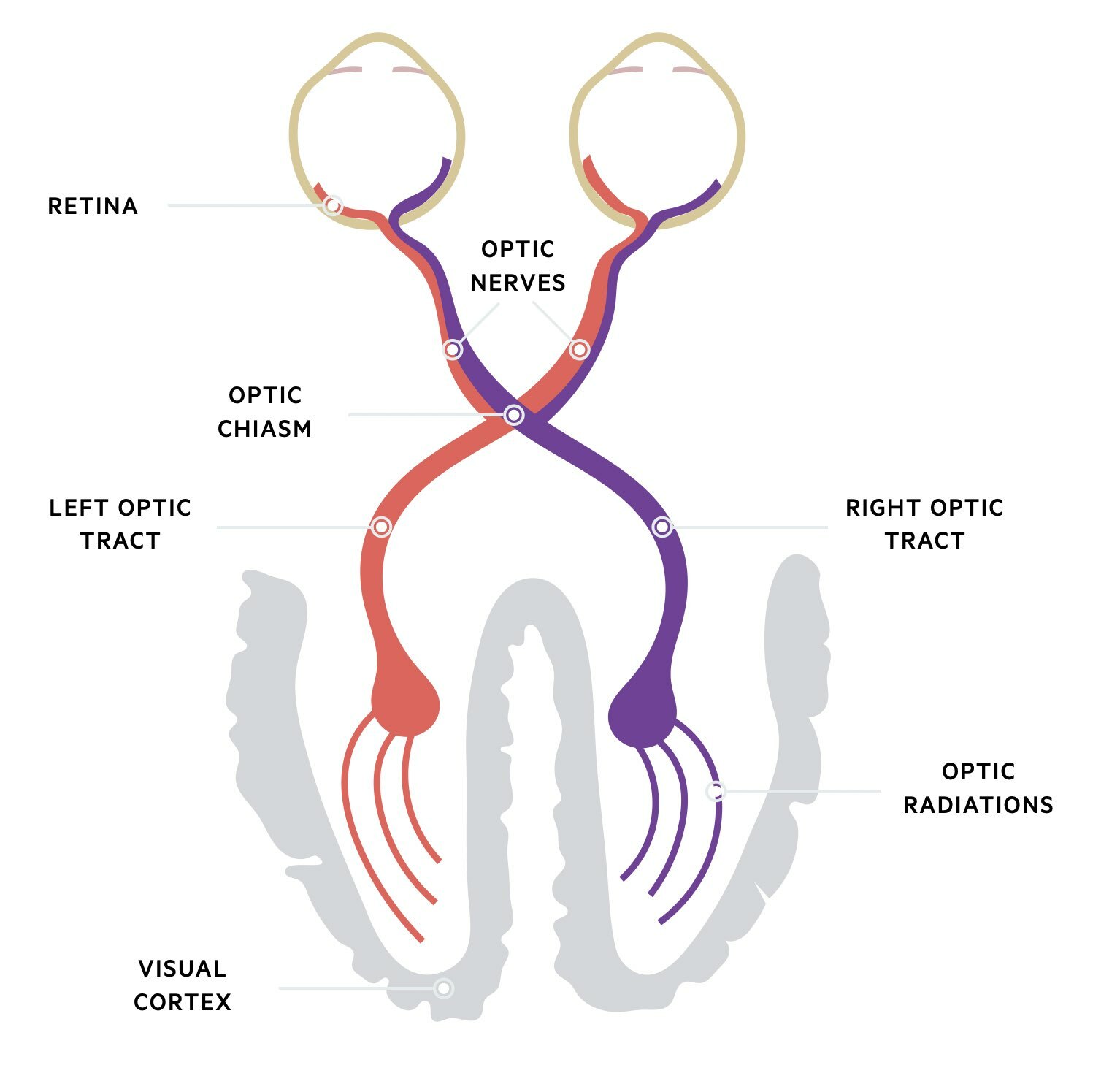
Retina
Specialised photoreceptors, known as rods and cones, are located within the retina. They are stimulated by light entering the eye and transmit information to retinal bipolar cells, which are a type of interneuron that connect photoreceptors to retinal ganglion cells. Consequently, bipolar cells transmit signals to these ganglion cells that converge at the optic disc. The axons of the retinal ganglion cells form the optic nerve.
Optic nerve
Sensory information is passed along the optic nerve, through the optic canal, to the optic chiasm to join the contralateral optic nerve.
Optic chiasm
The optic chiasm is formed by the joining of the paired optic nerves. Nasal retinal fibres cross at the optic chiasm to join the contralateral temporal retinal fibres.
Optic tract
Posterior to the optic chiasm the visual pathway continues as the right and left optic tracts. These tracts pass posteriorly to synapse with the lateral geniculate body within the midbrain. This structure is considered an extension of the thalamus.
The right optic tract corresponds to the left visual field and the left optic tract corresponds to the right visual field.
Optic radiations
Neurons from the lateral geniculate body pass dorsally towards the calcarine sulcus on the medical aspect of the occipital lobe. These fibres are collectively known as the optic radiations or geniculocalcarine tract (i.e. running from the geniculate body to calcarine sulcus) and can be divided into two loops:
- Upper (Baum’s): runs through the parietal lobe. Corresponds to the inferior visual field
- Lower (Meyer’s): runs through temporal lobe. Corresponds to the superior visual field
Visual cortex
Fibres from the optic radiations terminate within visual nuclei in the occipital lobe that makes up the primary visual cortex. From the visual cortex, neural signals are sent to other parts of the brain (e.g. frontal lobe, parietal lobe, temporal lobe), to help interpret the visual information received (e.g. facial recognition).
Pre-chiasmal field defects
Pre-chiasmal field defects are due to abnormalities with the retina or optic nerve.
Pre-chiasmal visual field defects occur due to a lesion anterior to the optic chiasm. These visual field defects are unilateral. They commonly occur due to damage of the retina or optic nerve and typically present with a scotoma or unilateral anopia.
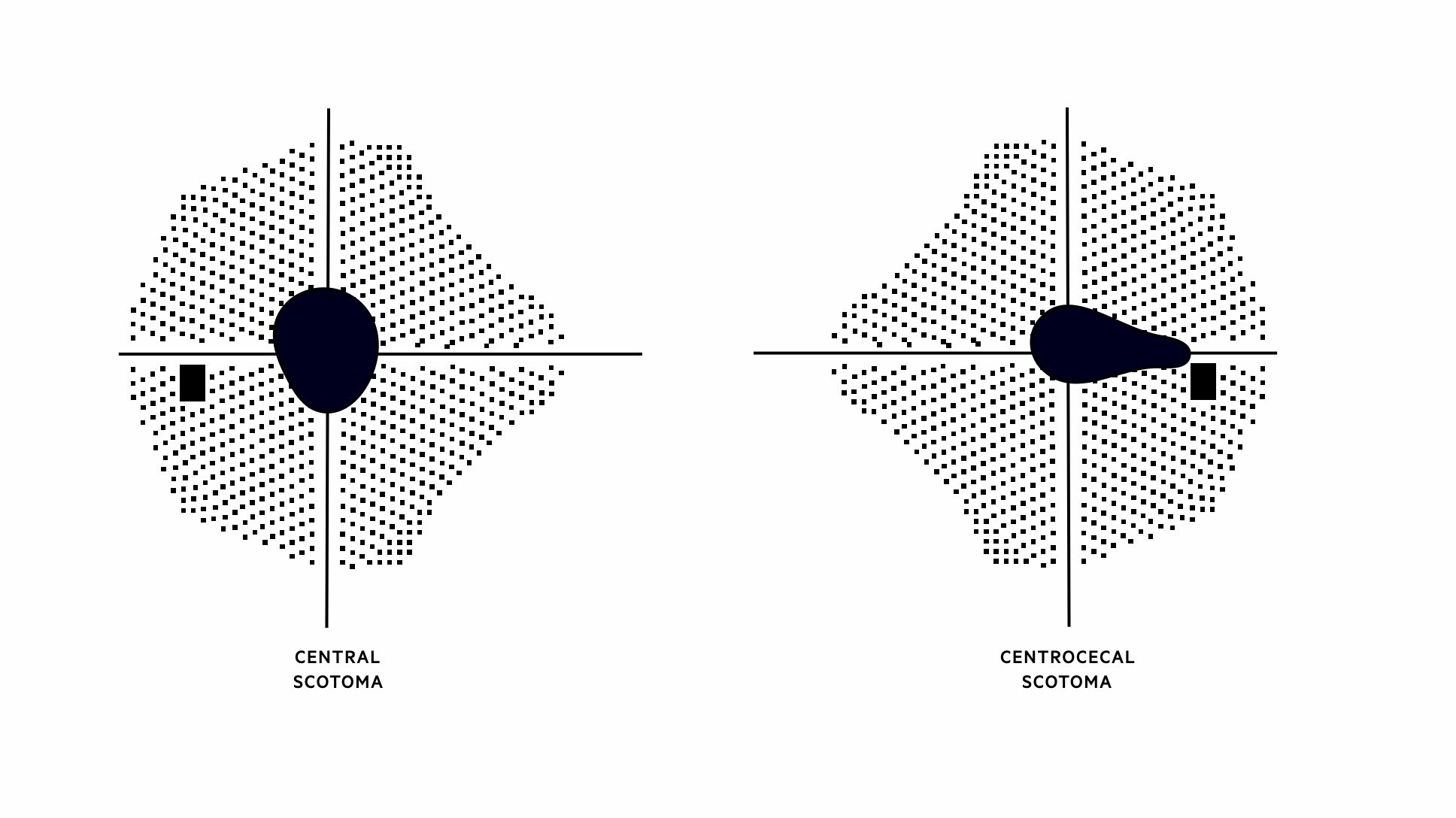
Scotoma
These refer to an area of reduced (or absent) vision in an otherwise normal visual field. The blind spot due to the optic nerve is an example of a physiological scotoma. Different types of scotoma can develop depending on the pattern of field loss (e.g. central, arcuate, centrocecal). A central scotoma involves the macula leading to a defect in central vision. Abnormalities of the peripheral retina, such as retinal detachment, can lead to a peripherally enlarging scotoma.
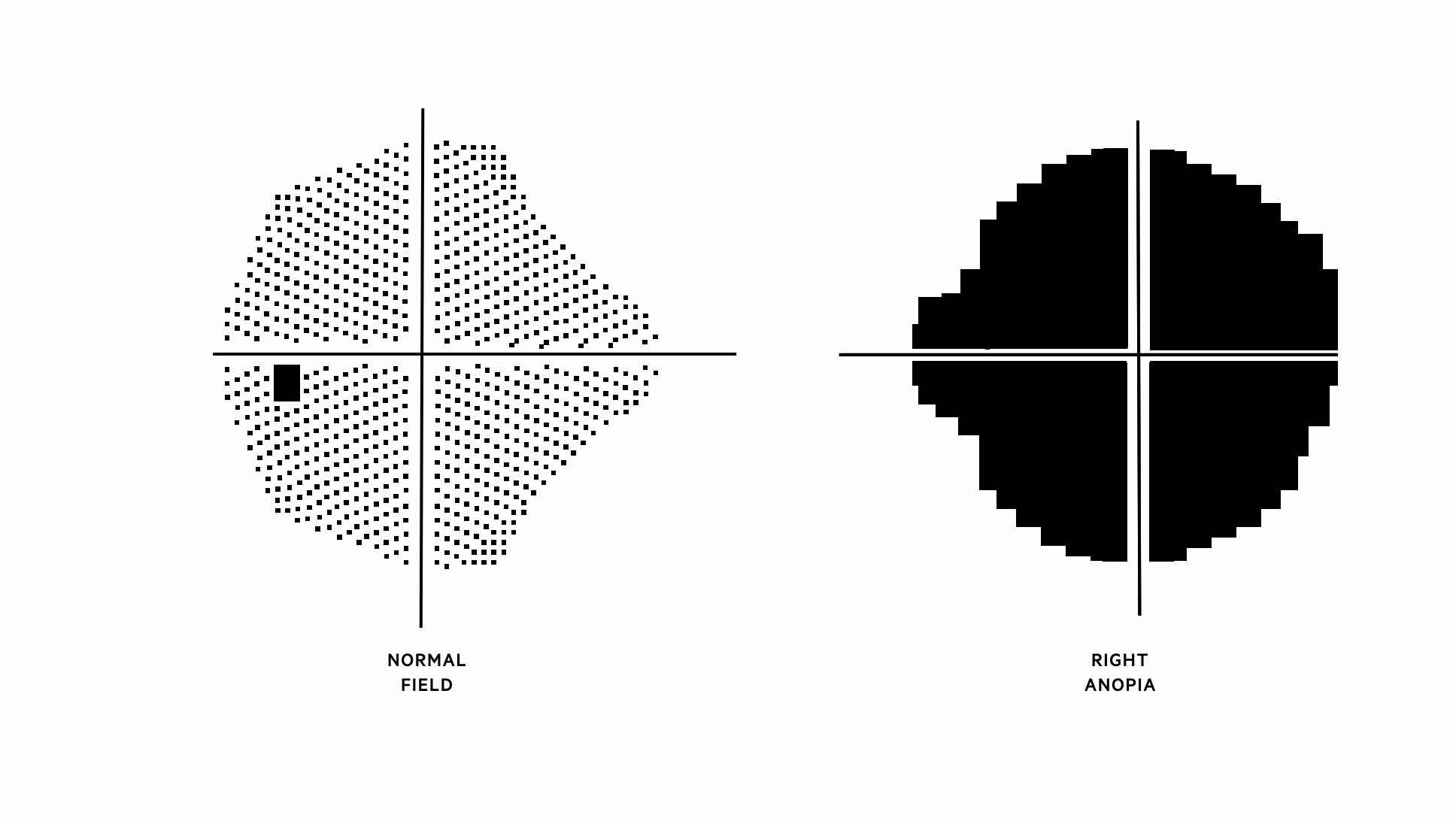
Anopia
This refers to the absence of sight. When it occurs in one-half of vision it is known as hemianopia. Complete anopia refers to the complete absence of vision. In pre-chiasmal field defects, anopia is unilateral. If there is damage to the optic nerve then complete unilateral anopia can develop.
Optic chiasm field defects
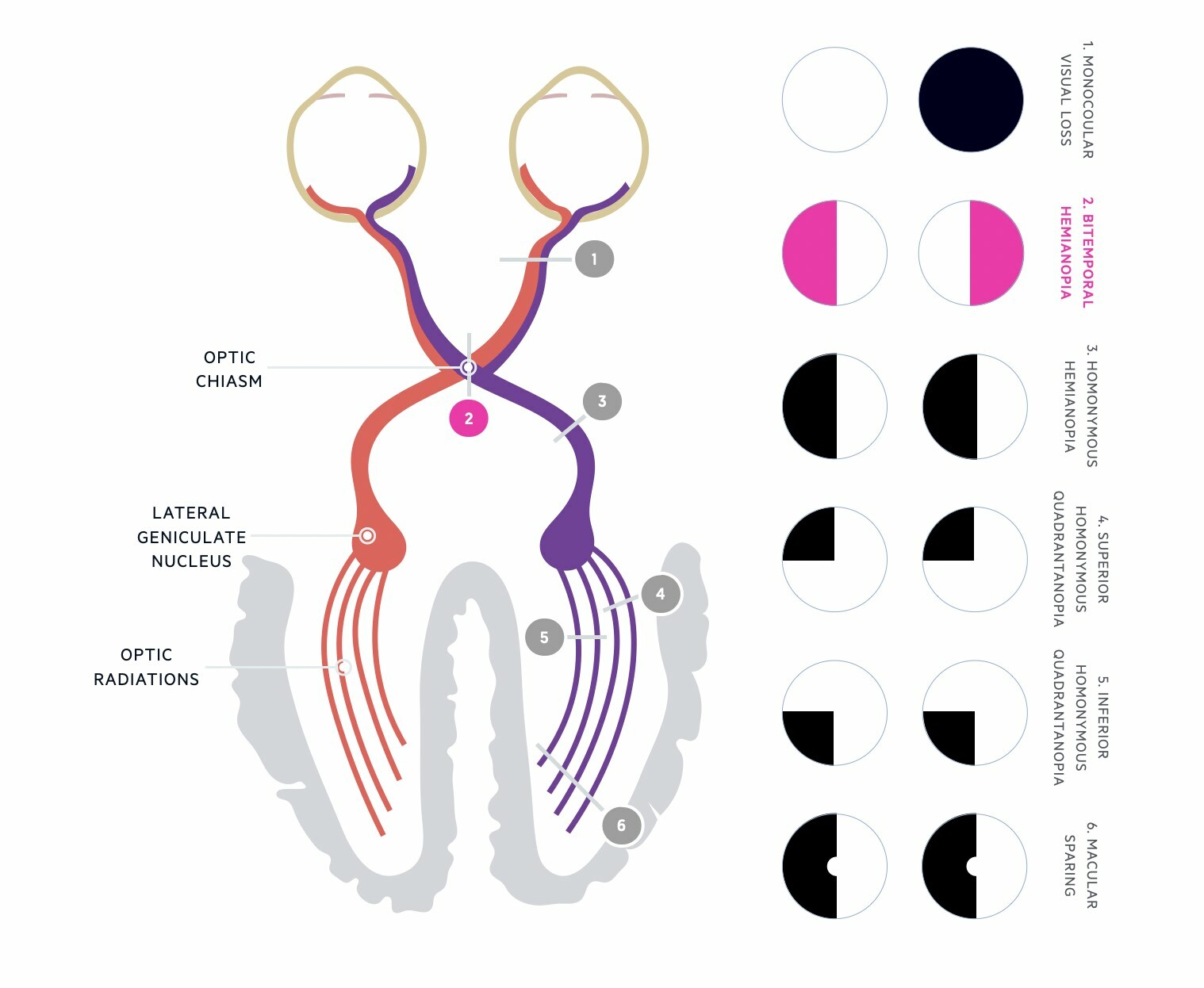
Lesions at the optic chiasm are characterised by bitemporal hemianopia.
Visual field defects may occur due to damage or compression of the optic chiasm. This causes a very classic visual field defect known as bitemporal hemianopia due to the crossing of nasal retinal fibres. There is a loss of vision in both temporal fields (the outer half of the visual field). A pituitary tumour is commonly the cause of bitemporal hemianopia due to its close proximity and subsequent compression of the optic chiasm.
Post-chiasmal field defects
Disruption at specific points within the visual pathway can lead to characteristic visual field defects.
Post-chiasmal field defects may occur from a lesion anywhere along the visual pathway from the optic chiasm to the visual cortex in the occipital lobe. These visual defects are bilateral. These types of field defects are most commonly associated with stroke due to disruption of the blood supply to the optic radiations or occipital cortex.
Homonymous hemianopia
Homonymous hemianopia refers to a visual field defect involving either the two right or the two left halves of the visual fields of both eyes. Vascular causes such as cerebral infarction or cerebral haemorrhage are the most commonly identified causes. In children, this visual field defect is commonly the result of a tumour.
Right homonymous hemianopia is due to a lesion on the left side of the brain and vice versa.
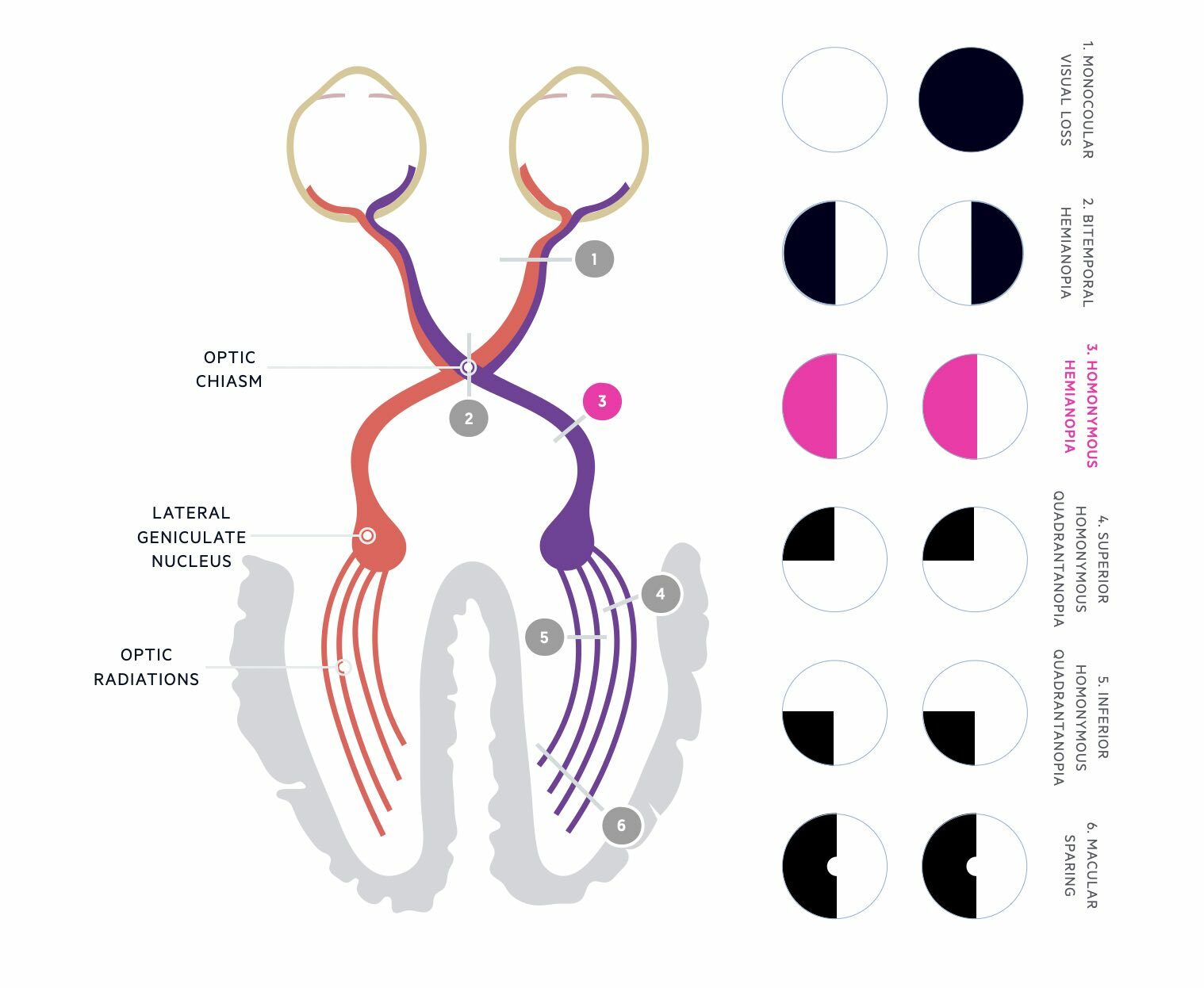
Superior homonymous quadrantanopia
A visual field defect involving the two right or two left upper quadrants of the visual fields in both eyes. Classically due to a lesion involving the temporal lobe optic radiations. Causes may include stroke, tumour, or demyelination. Accompanying features may include aphasia, memory deficits complex seizures, and auditory and visual hallucinations (depending on the dominance of the lobe).
A left superior homonymous quadrantanopia is due to a lesion on the right side of the brain (e.g. right temporal lobe)
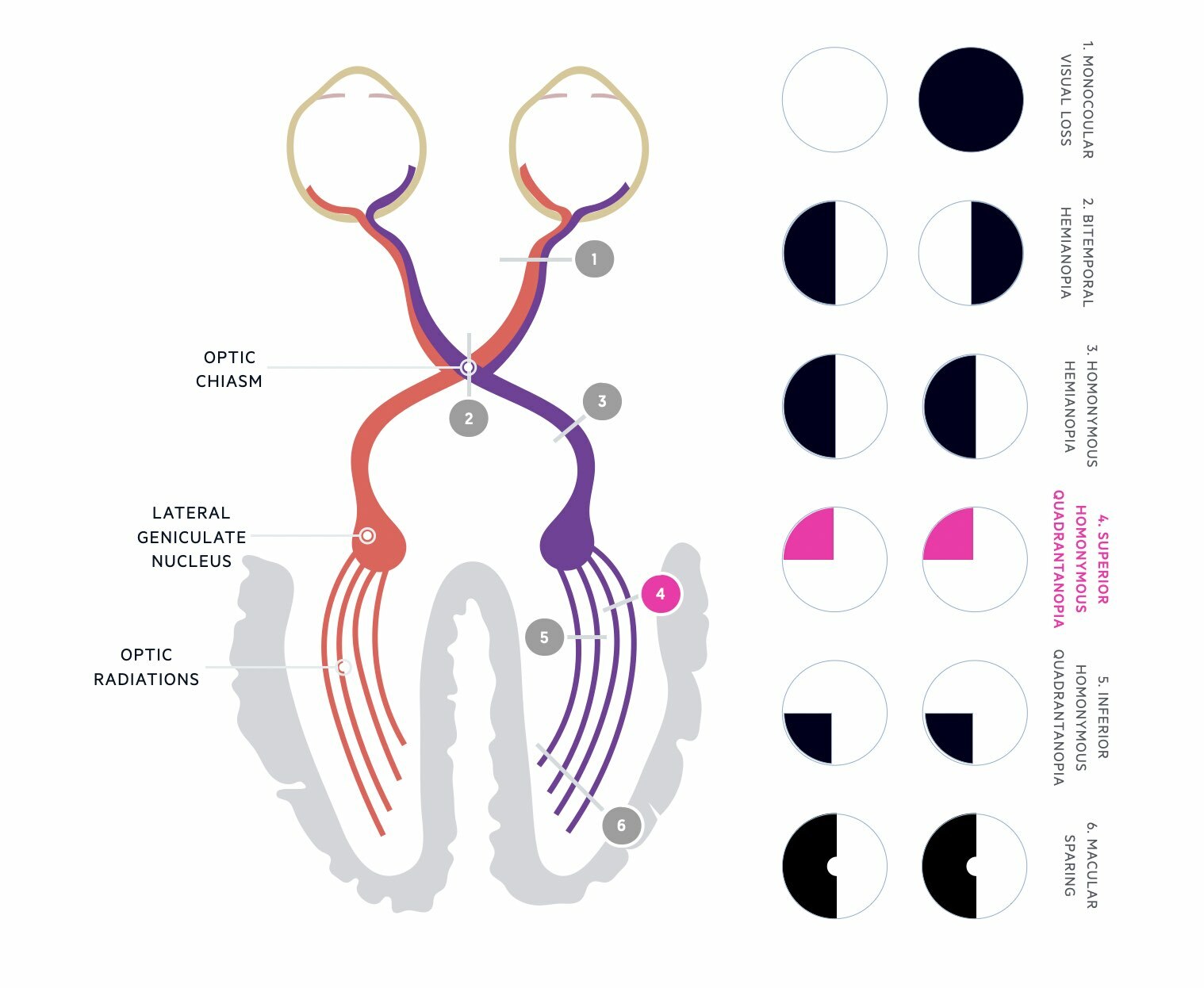
Inferior homonymous quadrantanopia
A visual field defect involving the two right or two left lower quadrants of the visual fields in both eyes. Classically due to a lesion involving the parietal lobe optic radiations. Causes may include stroke, tumour, or demyelination. Accompanying features may include finger agnosia (inability to identify specific fingers), acalculia (inability to perform simple cautions), and right-left disorientation, neglect and inattention (depending on the dominance of the lobe).
A left inferior homonymous quadrantanopia is due to a lesion on the right side of the brain (e.g. right parietal lobe)
Macular sparing
Lesions of the occipital lobe are the most common cause of homonymous hemianopia and are usually due to vascular disease (e.g. cerebral infarction or cerebral haemorrhage). Classically a lesion of the occipital lobe causes isolated homonymous hemianopia (e.g. right occipital lobe infarct causes left homonymous hemianopia) with macular sparing.
Macular sparing refers to the preservation of central vision. The reason for this is thought to be due to bilateral representation of the macula in the occipital cortex (i.e. the macular receives input from both the right and left occipital lobes).