What is open TMJ surgery?
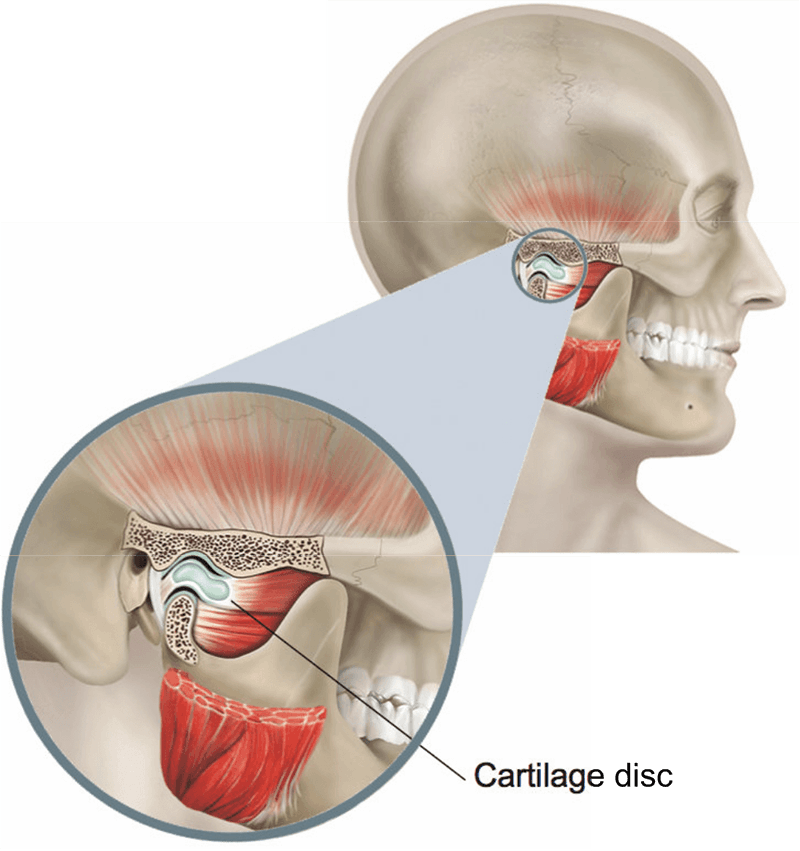
Open TMJ surgery allows your surgeon to see inside your temporomandibular joint (TMJ, or jaw joint) through a cut on your skin.
Your surgeon can diagnose and treat problems such as a torn cartilage and damage to the surface of the joint. They will be able to remove or change the position of the cartilage disc and reshape the lower and upper joint surfaces.
What are the benefits of surgery?
The aim is to confirm exactly what the problem is and to treat the problem at the same time.
Are there any alternatives to open TMJ surgery?
Problems inside a joint can often be diagnosed using tests such as CT scans and MRI scans.
Non-surgical treatment such as rest, taking anti-inflammatory painkillers and wearing a TMJ splint can usually help.
If the problem is with the chewing muscles around the joint, muscle-relaxing medication or injections of Botox can reduce joint stiffness but do not treat the underlying cause.
A steroid injection into the joint can sometimes reduce pain for several months but may cause side effects if repeated too often.
What does the operation involve?
The operation is performed under a general anaesthetic and usually takes about an hour for each joint.
Your surgeon will make a cut in front of your ear so they can open and examine the joint:
- If the cartilage disc is out of place, your surgeon will use stitches or put a small metal pin in the bone to hold the disc in place.
- If the disc itself is damaged, your surgeon will remove it. They may replace the disc using tissue from other areas of your body such as your ear or a nearby muscle in your temple.
- If a joint surface is damaged, your surgeon may reshape it, making it smoother.
- If your jaw keeps on coming out of joint, your surgeon may need to remove part of the upper joint surface.
Your surgeon will close the cuts with stitches. The stitches may be dissolvable.
How can I prepare myself for the operation?
If you smoke, stopping smoking now may reduce your risk of developing complications and will improve your long-term health. Stopping smoking and keeping your mouth clean significantly reduces the risk of infection.
Try to maintain a healthy weight. You have a higher risk of developing complications if you are overweight.
Regular exercise should help to prepare you for the operation, help you to recover and improve your long-term health. Before you start exercising, ask the healthcare team or your GP for advice.
Speak to the healthcare team about any vaccinations you might need to reduce your risk of serious illness while you recover. When you come into hospital, practise hand washing and wear a face covering when asked.
What complications can happen?
Some complications can be serious and can even cause death.
General complications of any operation
- bleeding
- bruising and swelling
- infection of the surgical site (wound)
- allergic reaction to the equipment, materials or medication
- blood clot in your leg
- blood clot in your lung
- chest infection
Specific complications of this operation
- continued pain for up to 6 months
- not being able to open your mouth fully (trismus) and jaw stiffness
- tenderness and pain in the joint
- numbness of the temple and ear
- weak forehead movement
- change in hearing
Consequences of this procedure
- pain
How soon will I recover?
The swelling and discomfort is usually at its worst after about 2 days.
You should be able to go home the same day or the day after.
If the stitches are not dissolvable, they are usually removed after 4 to 6 days.
Regular exercise should help you to return to normal activities as soon as possible. Before you start exercising, ask the healthcare team or your GP for advice.
It is important to keep the joint moving. Your surgeon will give you stretching exercises to do to help improve how your mouth opens. You should continue to rest and wear any splints until you are told otherwise.
You should be able to return to work after a few days, depending on your type of work.



