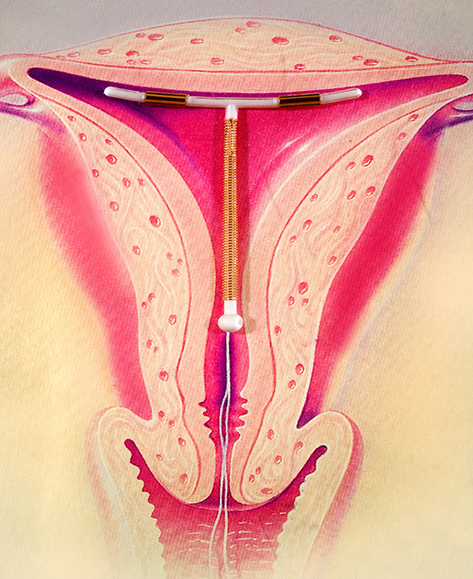
Intrauterine contraceptive device (IUD)
What is an intrauterine device (IUD)?
An intrauterine device (IUD) is a type of contraception (birth control).
IUDs are small devices that are placed inside the uterus (womb) to prevent pregnancy. There are 2 types of IUD:
- the hormonal IUD
- the copper IUD
An IUD needs to be put in place by a trained doctor or nurse.
How does an IUD work to prevent pregnancy?
IUDs are highly effective and reliable. They last for 5 years or more.
The hormonal IUD
Hormonal IUDs are made of plastic and slowly release a progestogen hormone called levonorgestrel.
The hormonal IUD prevents pregnancy by:
- thickening the mucus at the entrance to the uterus so sperm cannot get through
- making it harder for sperm to reach and fertilise an egg
- making it harder for an egg to survive
- thinning the lining of the uterus
- preventing ovulation (the release of eggs from the ovaries) in some people
There are 2 brands of hormonal IUDs available in Australia:
- Mirena
- Kyleena
Hormonal IUDs work for up to 5 years. Kyleena contains a lower dose of hormone than Mirena.
You may need to use another form of contraception (birth control) for 7 days after having a hormonal IUD put in. Check with your doctor or nurse about this.
The copper IUD
The copper IUD is made of copper and plastic. It does not release any hormones.
The copper IUD works by:
- making it harder for sperm to reach and fertilise an egg
- making it harder for an egg to survive
- changing the lining of the uterus so that if an egg was fertilised, it wouldn’t be able to implant
There are 2 brands of copper IUD available in Australia — one lasts for up to 5 years and the other for up to 10 years.
The copper IUD can also be used as a type of emergency contraception if it is put in within 5 days of unprotected sex.
How effective is the IUD at preventing pregnancy?
The IUD works very well, and is one of the most effective methods of contraception available.
Fewer than 1 in 100 people using an IUD will become pregnant.
How is an IUD put in?
IUDs can only be inserted by a specially trained doctor or nurse.
When the IUD is put in, you are in a similar position to when you have a cervical screening test. An instrument called a speculum is placed in your vagina. Local anaesthetic can be used to reduce discomfort or pain.
For a couple of days after having an IUD inserted, you should avoid:
- using tampons or menstrual cups
- having sex
- having a bath
- swimming
You should check the IUD thread about once a month to make sure your IUD is still in place. You will be shown how to do this.
Are there any side effects with IUDs?
After having an IUD put in, you may have cramps and bleeding for a few days.
Ongoing hormonal IUD side effects can include:
- ovarian cysts
- headaches
- mood changes
- weight gain
- breast tenderness
- lowered interest in sex
- acne
When should I see my doctor?
If you’re experiencing troublesome IUD side effects after having an IUD put in, see your doctor.
See your doctor if cramps and bleeding continue for more than a few days after having an IUD put in.
See your doctor straight away if you have:
- an unusual vaginal discharge
- pain in your lower tummy
- pain during sex
What are the advantages and disadvantages of the IUD?
Advantages of both types of IUD:
- They are extremely good at preventing pregnancy.
- IUDs are easy to use and can stay in place for 5 to 10 years.
- IUDs are cost-effective.
- They can be used if you are breastfeeding.
- Your cycle and fertility return quickly when the IUD is removed.
Hormonal IUDs, especially the Mirena, can also help with heavy periods and period pain. Sometimes your periods stop altogether.
Disadvantages of IUDs include:
- They need to be inserted by a doctor or nurse.
- There is a small risk with insertion, such as difficulty with insertion, pain or discomfort, damage to the uterus and infection.
- An IUD can move out of place and sometimes come out by itself.
- Hormonal IUDs can cause side effects such as irregular vaginal bleeding or spotting.
- Copper IUDs can make periods heavier and longer and cause spotting.
- IUDs do not protect against sexually transmitted infections (STIs).
An IUD is not suitable for everyone. Talk to your doctor or go to your local family planning clinic for advice on whether an IUD may be a good option for you.
How is an IUD taken out?
IUD removal is a quick procedure. Your doctor or nurse will gently pull on the IUD string to take it out. The IUD’s arms fold up so that it slips out.
Some women find the procedure uncomfortable while others don’t feel very much.
You can have a new IUD inserted at the same visit. If you are changing to another type of contraception, talk to your doctor about your options.


