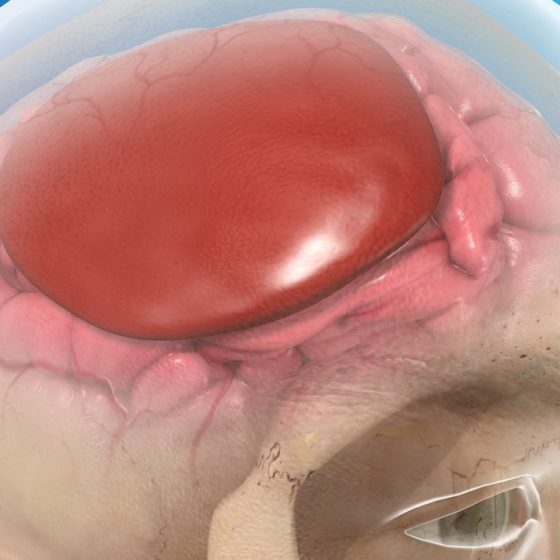
Lymphadenopathy
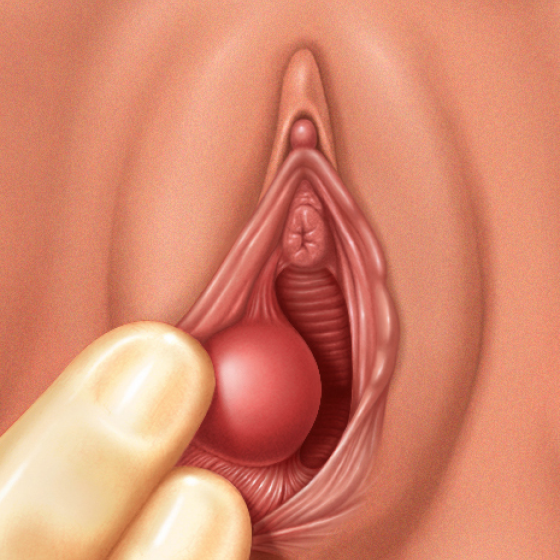
Overview Lymphadenopathy essentially refers to lymph nodes with abnormal consistency or size. Lymphadenopathy is a very broad term that simply refers to the disease of lymph nodes. The term is used to represent a change in size or consistency of a lymph node. The two most common causes of lymphadenopathy are infection and malignancy. Lymphadenopathy may be peripheral or visceral: Peripheral: lymph nodes located in areas close to the skin that can be palpated when enlarged (e.g. neck, axilla, groin) Visceral: lymph nodes located inside the body at deep locations, usually in association with major organs (e.g. mesenteric lymph nodes,